- Review
- Open access
- Published:
The past, present and future of anti-malarial medicines
Malaria Journal volume 18, Article number: 93 (2019)
Abstract
Great progress has been made in recent years to reduce the high level of suffering caused by malaria worldwide. Notably, the use of insecticide-treated mosquito nets for malaria prevention and the use of artemisinin-based combination therapy (ACT) for malaria treatment have made a significant impact. Nevertheless, the development of resistance to the past and present anti-malarial drugs highlights the need for continued research to stay one step ahead. New drugs are needed, particularly those with new mechanisms of action. Here the range of anti-malarial medicines developed over the years are reviewed, beginning with the discovery of quinine in the early 1800s, through to modern day ACT and the recently-approved tafenoquine. A number of new potential anti-malarial drugs currently in development are outlined, along with a description of the hit to lead campaign from which it originated. Finally, promising novel mechanisms of action for these and future anti-malarial medicines are outlined.
Background
In 2017, the World Health Organization (WHO) estimated that there were 219 million cases of malaria worldwide, an increase of 2 million from the previous year, and as a result there were 435 thousand deaths, or 1190 per day, mostly young children [1]. Encouragingly, since 2000, these figures have decreased by about 37% worldwide, but a number of recent reports have shown that this level is slowly plateauing, emphasizing that there must not be complacency with the current treatment and prevention strategies [2, 3]. There are five species of the Plasmodium parasite, with Plasmodium falciparum being the most prevalent in Africa and Plasmodium vivax being the most prevalent in countries outside Africa. Almost half the world’s population is at risk of contracting malaria, with Africa having the biggest share of cases and deaths of any continent (\(\sim\) 90%).
Over the past few years, a number of reviews have been published which evaluate the potential future of anti-malarial drugs. Of note: Triple-anti-malarial drug combinations were examined in 2014 [4]; a review on the numerous strategies currently used in anti-malarial drug discovery was published in early 2017 [5], and an in-depth primer on all aspects of malaria was published in late 2017 [6]. In early 2018, a review was published highlighting the discovery and development of a number of new anti-malarial drug candidates [7, 8].
This review aims to summarize the past, present and future of compounds used to treat malaria. There is a focus on projects supported by the Medicines for Malaria Venture (MMV), a non-governmental organisation that maintains a website [9] highlighting collaborations from the very early stages of drug discovery and lead optimization (e.g. the Open Source Malaria (OSM) project with which the authors are involved [10]), to the progression of lead compounds through clinical trials (e.g. Cipargamin, which has been developed by Novartis [11]) and all the way to the final stages of bringing a drug to market (e.g. Artesunate for injection, developed by Guilin Pharmaceutical). After a brief survey of past medicines, and those that are currently being used, focus will be put on compounds that are currently in development, and in particular the lead optimization campaigns of each. Since it is such a crucial component of modern anti-malarial drug discovery, this review will end with a survey of the most promising mechanisms of action of those compounds in development.
The scope of this review encompasses compounds described by the MMV survey of current anti-malarials, previous reviews on anti-malarial drugs, as well as compounds currently undergoing active clinical trials. The information presented in this review was obtained through structure searching of the relevant compounds in the SciFinder database. Additional references were found through the Web of Science database (Additional file 1).
Past
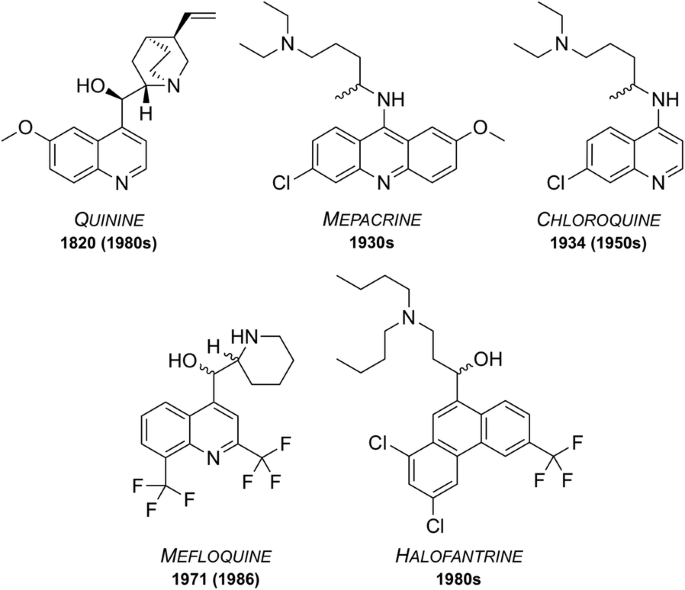
Since the isolation in 1820 of quinine, the first chemically purified effective treatment for malaria, a number of other natural and synthetic compounds have been developed (Fig. 1). However, as time passed, strains of the parasite began to show signs of resistance towards these drugs, rendering them less effective. Accordingly, their use has ceased or is restricted to particular situations.
Quinine
First isolated from the bark of the cinchona tree in 1820, quinine has been used as one of the most effective treatments for malaria to date [12]. Resistance was first reported in the 1980s [13] and as of 2006, quinine is no longer used as a front-line treatment for malaria but is still on the WHO’s Model List of Essential Medicines (MLEM) [14] for the treatment of severe malaria in cases where artemisinins are not available.
Mepacrine
Mepacrine (a.k.a quinacrine) was predominantly used throughout the Second World War as a prophylatic, sold under the trade name Atabrine [15]. This compound is a derivative of methylene blue, another anti-malarial that was discovered in 1891 and found to be an effective treatment for malaria [16, 17]. Its use has declined over the years but methylene blue and its derivatives are, however, the subject of increasing current interest [18] and it is currently in clinical trials as a combination with primaquine (vide infra). Mepacrine itself is no longer used today due to the high chance of undesirable side effects such as toxic psychosis [19].
Chloroquine
During the 1940s, chloroquine (CQ) was used to treat all forms of malaria with few side effects [20]. Resistance to CQ was first reported in the 1950s and over the years many strains of malaria have developed resistance. Indeed, resistant strains (K1, 7GB, W2, Dd2, etc.) of the malaria parasite are now used in potency evaluation assays as a way of showing efficacy [21]. Chloroquine is on the MLEM for the treatment of P. vivax in regions where resistance has not developed [14].
Mefloquine
Mefloquine was developed in the 1970s by the United States Army [22] and is still used today, also being one of the medicines on the MLEM. Originally introduced for the treatment of chloroquine-resistant malaria, it has been used as both a curative and a prophylactic drug. Resistance was first reported in 1986 [23]. It is thought that the structurally related quinoline drugs (such as quinine, mepacrine, chloroquine and mefloquine) act through the disruption of haemoglobin digestion in the blood stage of the parasite [24]. These drugs are commonly used in combination with a complementary drug (e.g. mefloquine and artesunate, sold as Artequin™) to reduce the chance of resistance development to the quinoline family of compounds. Mefloquine is commonly sold in its racemic form under the brand name Lariam®, however it is no longer widely used due to the perception of central nervous system toxicity that has been suggested to affect a large number of its users [25].
Halofantrine
Developed between the 1960s and 1970s by the Walter Reed Army Institute of Research [26], halofantrine was initially used for treatment against all forms of the Plasmodium parasite. Its use has diminished over time due to a number of undesirable side effects, such as the potential for high levels of cardiotoxicity. It is only used as a curative drug and not for prophylaxis due to the high toxicity risks and its unreliable pharmacological properties. Halofantrine is still used today, under the brand name Halfan™, but only in cases where patients are known to be free of heart disease and where infection is due to severe and resistant forms of malaria [27].
Present
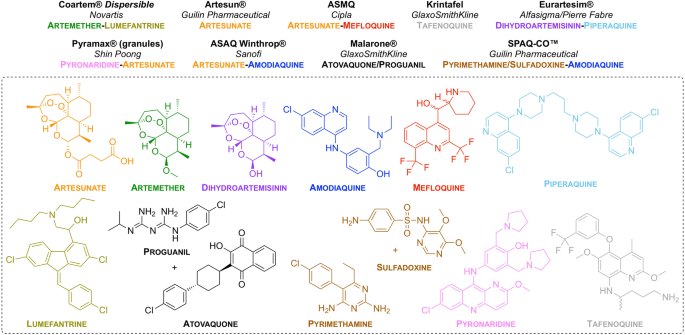
On the WHO Model List of Essential Medicines [14], there are currently listed 14 medicines for curative treatment of malaria and 4 medicines for prophylactic treatment, with the treatments formulated either as single compounds or as combinations. Perhaps the most effective of these are the artemisinin-based combinations which use an artemisinin derivative (short-acting) in combination with one or more complementary compounds (long-acting and possessing different mechanisms of action).
MMV have been involved in progressing nine new anti-malarial treatments based on different formulations/combinations of approved drugs (Fig. 2). All of these compounds are on the MLEM as combination therapies.
Artemisinin and its derivatives
Artemisinin was first isolated in 1971 by Tu Youyou from the plant Artemisia annua, a herb that has commonly been used in Chinese traditional medicine [28]. Due to the great positive impact of artemisinin in combating malaria, Youyou was awarded the joint Nobel Prize in Physiology or Medicine in 2015 for “her discoveries concerning a novel therapy against malaria” [29]. Artemisinin has been shown to be efficacious against all multi-drug resistant forms of P. falciparum. The most common derivatives of artemisinin are artemether, artesunate and arteether. These semi-synthetic derivatives are prodrugs which are transformed to the active metabolite, dihydroartemisinin. The use of artemisinins has been integral in the fight against malaria with ACT making up the majority of modern day treatments [30]. Although slow to develop, the first report of resistance to artemisinin was in western Cambodia in 2008 [31]. Ten years later, in February of 2018, a report was published identifying more than 30 independent cases of artemisinin resistance in southeast Asia, specifically with resistance to the dihydroartemisinin–piperaquine combination therapy [32].
The mechanism of action (MoA) through which artemisinin acts has been widely debated [33]. The most accepted theory is that the molecule is activated by haem to generate free radicals, which in turn damage proteins required for parasite survival [34, 35]. Still, evidence for a number of other possible mechanisms have been found. In 2013, a computational approach was taken to determine the MoA based around previous studies which identified haem and PfATP6 (Ca2+ transporter) as potential MoAs [36]. More recently in 2015, artemisinin was shown to be associated with the up-regulation of the unfolded protein response (UPR) pathways which may be linked to decreased parasite development [37]. Another study showed that artemisinin was is a potent inhibitor of P. falciparum phosphatidylinositol-3-kinase (PfPI3K) [38].
Amodiaquine
Amodiaquine was first synthesized in 1948 [39]. It is mainly used for the treatment of uncomplicated P. falciparum malaria when used in combination with artesunate and is commonly sold under the trade name Camoquine® or Coarsucam™ [40]. Similar to chloroquine, amodiaquine’s MoA is thought to involve complexation with haem and inhibition of haemozoin formation [41].
Piperaquine
Piperaquine was developed in the 1960s as a part of the Chinese National Malaria Elimination Programme [42]. Initially used throughout China as a replacement for chloroquine, resistance led to its diminished use as a monotherapy. While the MoA of piperaquine is not completely understood, studies have suggested that it acts by accumulating in the digestive vacuole and inhibiting haem detoxification through the binding of haem-containing species [30, 43]. These days, piperaquine is used as a partner drug with dihydroartemisinin (commonly sold under the trade name Eurartesim®).
Lumefantrine
Lumefantrine (a.k.a. benflumetol) was first synthesized in 1976 as a part of the Chinese anti-malarial research effort “Project 523” which also resulted in the discovery of artemisinin [44]. It is currently sold under the trade name Coartem®. The exact MoA of lumefantrine is unknown, however studies suggest that it inhibits nucleic acid and protein synthesis through the inhibition of \(\beta\)-haematin formation by complexation with haemin [41]. Lumefantrine is currently used only in combination with artemether.
Proguanil and atovaquone
Proguanil was first reported in 1945 as one of the first antifolate anti-malarial drugs [45], while atovaquone was first reported in 1991 for the treatment of protozoan infections [46]. The combination of these, commonly sold as Malarone™, has been marketed by GlaxoSmithKline (GSK) since the early 2000s, and has proven to be a very effective anti-malarial due to the synergistic effect of the two components. This is, in large part, due to the different MoAs for each compound. Atovaquone acts as a cytochrome bc\(_\text {1}\) complex inhibitor which blocks mitochondrial electron transport [47]. Proguanil (when used alone) acts as a dihydrofolate reductase (DHFR) inhibitor through its metabolite, cycloguanil (CG) which disrupts deoxythymidylate synthesis. When used in combination with atovaquone however, proguanil does not act as a DHFR inhibitor but has instead been shown to reduce the concentration of atovaquone required for treatment [48]. Generic atovaquone/proguanil is still available today for the treatment of chloroquine-resistant malaria.
Pyrimethamine and sulfadoxine
Pyrimethamine (PYR) was developed in the early 1950s by Gertrude Elion and George Hitchings and is now sold under the trade name Daraprim™ [49]. The development of pyrimethamine was a part of the efforts that won Elion, Hitchings and Black the joint Nobel Prize in Physiology or Medicine in 1988 for “their discoveries of important principles for drug treatment” [50]. Sulfadoxine was developed in the early 1960s [51]. It is no longer used as a preventative drug due to high levels of resistance. The combination of pyrimethamine and sulfadoxine was approved for use for the treatment of malaria in 1981 and is now commonly sold under the trade name Fansidar®. Both drugs are known to target the parasite folate biosynthesis pathway [52]. Pyrimethamine inhibits dihydrofolate reductase, while sulfadoxine inhibits dihydropteroate synthetase.
Pyronaridine
Pyronaridine was first synthesized in the 1970s at the Institute of Chinese Parasitic Disease [53, 54]. It has been found to be efficacious against chloroquine resistant strains and has been in use for over 40 years, sold under the trade name Pyramax® (in combination with artesunate). Like lumefantrine, pyronaridine has been found to act through the inhibition of \(\beta\)-haematin formation [55].
Tafenoquine
First discovered in 1978 at the Walter Reed Army Institute of Research, Tafenoquine (TQ) was recently approved by the United States Food and Drug Administration for use as the first new single-dose for the radical treatment of P. vivax malaria in over 60 years [56]. TQ is thought to be a prodrug which is metabolized to the active quinone TQ, however the MoA is not well known [57]. It is currently sold under the brand name Krintafel.
Future
(Adapted from the MMV-supported projects webpage [58])
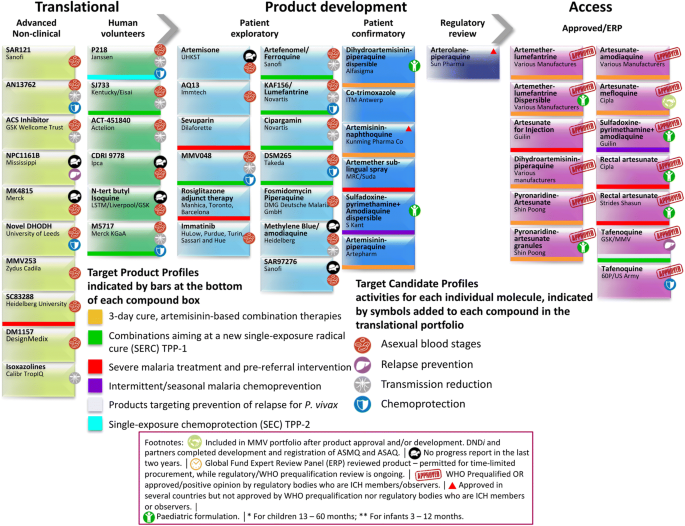
Snapshot of the projects supported by MMV at different stages of the drug discovery and development pipeline
Since its establishment in 1999, the Medicines for Malaria Venture has been frontlining the discovery and development of new medicines for the treatment of malaria. The potential for these compounds to act as new anti-malarials is judged by a number of requirements: novel modes of action with no cross-resistance to current drugs; single-dose cures (artesunate and chloroquine are unable to do this); activity against both the asexual blood stages that cause disease and the gametocytes responsible for transmission; compounds that prevent infection (chemoprotective agents); and compounds that clear P. vivax hypnozoites from the liver (anti-relapse agents) [59, 60]. MMV has been aiding the fight against malaria by partnering with universities and pharmaceutical companies around the world to bring new anti-malarials to market (Fig. 3).
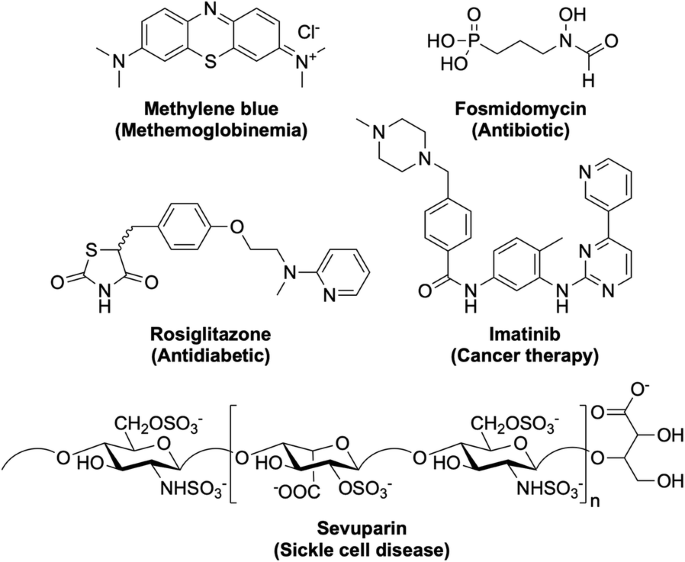
Besides the traditional drug discovery and development methods for the identification of new anti-malarials that will be described below, there are a number of other ways in which a new anti-malarial drug may be discovered. One way, as previously mentioned, is through the exploration of new combinations and formulations of current anti-malarial drugs. This may help overcome issues with resistance to a particular component or may assist in the delivery of the drug allowing it to be more effective. Alternatively, existing drugs used for other purposes may be found efficacious against malaria and subsequently be repurposed as a new anti-malarial treatment. This can be advantageous since these compounds may have already shown good biological properties and may also reveal novel MoAs. Examples include those shown in Fig. 4.
Methylene blue, a drug for the treatment of methaemoglobinemia. Last completed Phase II trials in 2017 (NCT02851108) as a combination with primaquine. Fosmidomycin, an antibiotic. Most recently in Phase II trials in 2015 (NCT02198807) as a combination with piperaquine. Rosiglitazone, an antidiabetic drug. Currently in clinical trials as an adjunctive therapy for severe malaria (NCT02694874). Imatinib, a cancer therapy drug. Currently in Phase II trials (NCT03697668) as a triple combination with dihydroartemisinin-piperaquine. Sevuparin, a drug for the treatment of sickle cell disease. Last in Phase I/II trials in 2014 (NCT01442168) as a combination with atovaquone-proguanil.
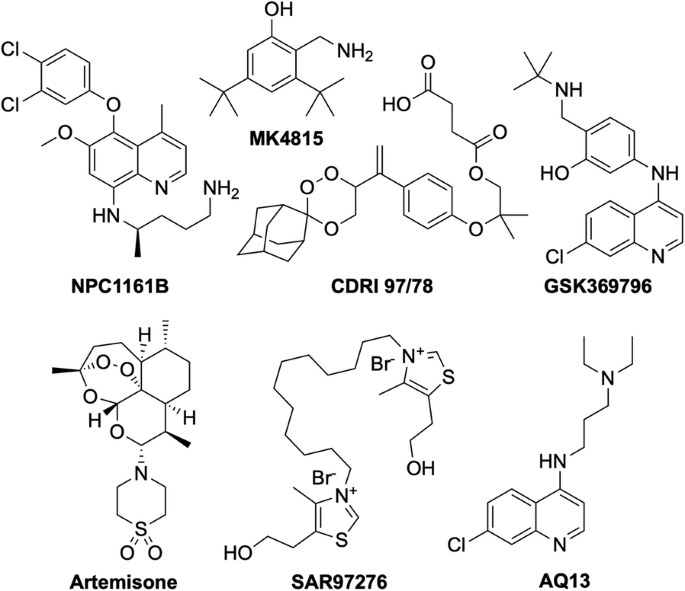
The following seven compounds were discovered and developed with the hope of progressing into clinical trials as potential new anti-malarial candidates (Fig. 5). However, over the past two years, progress in the development of these compounds has slowed, making the fate of these drug candidates less clear.
The chiral 8-aminoquinoline derivative, NPC1161B was developed at the University of Mississippi and was still in preclinical studies in 2014 [61,62,63,64]. MK4815 was developed in 2012 at Merck but is still in preclinical studies due to safety issues [65]. CDRI 97/78 is a fast-acting novel trioxane anti-malarial first synthesized in 2001 by a team at the Council of Scientific and Industrial Research in India [66]. Having passed all preclinical studies, it was last seen to have completed first-in-human Phase I trials in 2014 [67]. Developed at the Liverpool School of Tropical Medicine in 2009, N-tert butyl isoquine/GSK369796 was designed as an alternative to amodiaquine [68, 69]. It completed preclinical studies [70], and was last in Phase I trials in 2008 (NCT00675064). Artemisone is a second-generation semi-synthetic artemisinin derivative developed at the Hong Kong University of Science and Technology, that has previously been shown to be as efficacious as artesunate, with minimal neuro- and cytotoxicity and a comparably low cost of production [71]. It was withdrawn from Phase II/III trials in 2010 (NCT00936767). The bisthiazolium salt, SAR97276, was discovered and developed by Sanofi in 2005 [72], however further investigation was terminated in 2012 after Phase II trials (NCT01445938). AQ-13 is a chloroquine derivative that was first described in 1946 [73]. While only differing to CQ in the amine side-chain, this difference has been linked to its increased efficacy against CQ-resistant strains [74]. It has a MoA and pharmacokinetic properties similar to that of CQ [75, 76]. AQ-13 last completed Phase II trial at the end of 2017 (NCT01614964) [77], however there has been no mention of any following active trials so the ongoing status of this compound is unclear.
The compounds in the remainder of this section are currently still actively being pursued. For ease of visualisation throughout in this section, a graphical summary of each compound structure and its code will be displayed, along with key physical and biological properties identified during the hit to lead campaigns (Additional file 2).
Preclinical
Once a lead compound has been identified, optimization of the structure can begin. This largely involves investigation into the structure activity relationship (SAR) of the drug, optimising for properties such as potency (both in vitro and in vivo), solubility and metabolic stability. The candidate must also be assessed for any possible toxicity (e.g. dosing, cytotoxicity/genotoxicity levels, etc.).
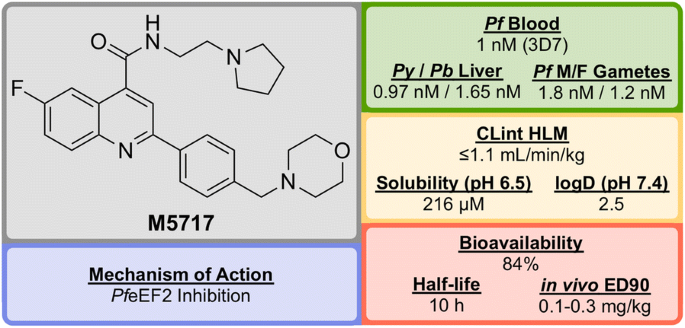
M5717 (Fig. 6) was developed in 2015 by a team led by the Drug Discovery Unit (DDU) in Dundee and was shown to have potent activity against multiple stages of the Plasmodium parasite via a novel mechanism of action [78, 79].
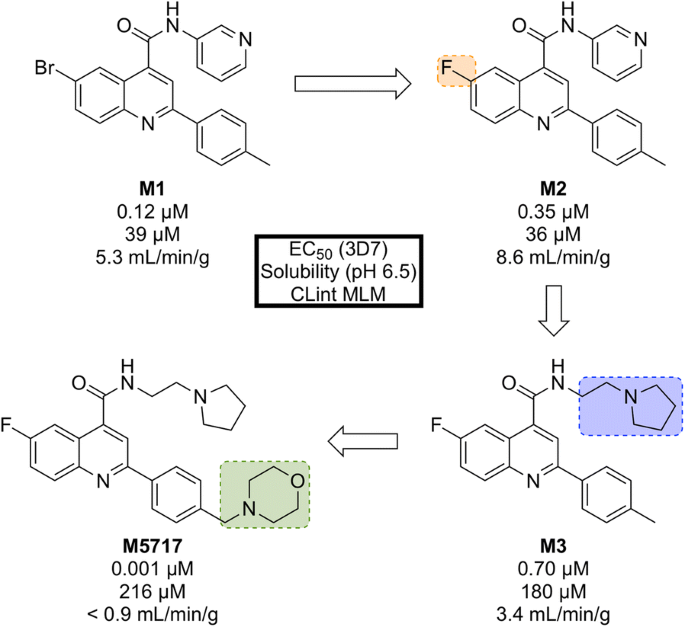
Initial phenotypic screening of the Dundee protein kinase scaffold library against the 3D7 multi-drug-resistant P. falciparum strain identified a compound (M1, Fig. 7) that possessed high potency against the parasite, albeit with poor physicochemical properties. Optimization of this structure (via M2 and M3) led to improvements across the board (M5717).
In addition to the nanomolar activity against the 3D7 strain, M5717 has shown almost equal potency against a number of other drug-resistant strains (K1, W2, 7G8, TM89C2A, D6 and V1/S) as well as similar potencies across multiple life cycle stages (liver schizonts, gametocytes and ookinetes).
M5717 was found to be as effective as current anti-malarial drugs (chloroquine, mefloquine, artemether, dihydroartemisinin and artesunate) when evaluated in the in vivo Plasmodium berghei mouse model for single-dose efficacy showing > 99% reduction in parasitaemia at doses of 4 \(\times\) 30 mg/kg p.o. q.d. and an ED\(_{90}\) of 0.1–0.3 mg/kg.
Due to its novel MoA (PfeEF2 inhibition, vide infra) and its ability to clear blood-stage parasites completely, M5717 satisfies the requirements to be a long duration partner and could be used as part of a combination therapy with a fast-acting compound [80]. Additionally, the compound has shown the ability to act as a transmission-blocking drug (stage IV–V) and also to be effective for chemoprotection.
In late 2017, M5717 was cleared for progression from development to Phase I clinical trials for volunteers in Australia (NCT03261401).
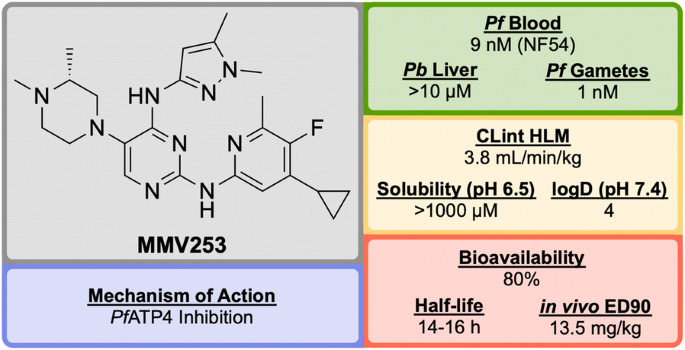
Identified by AstraZeneca in 2015, MMV253 (Fig. 8) is a novel triaminopyrimidine (TAP) that has shown good in vitro potency and in vivo efficacy, and acts through another novel MoA [81].
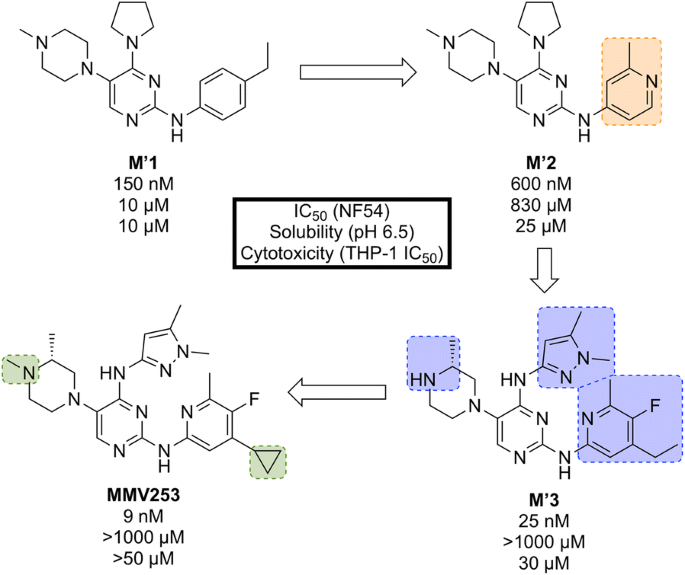
High-throughput screening of 500,000 compounds from AstraZeneca’s library against blood stage P. falciparum resulted in the identification of a promising series of TAPs. The initial hit (M’1, Fig. 9) suffered from hERG inhibition and poor solubility which, through lead optimization, was improved upon to give a compound that possessed high potency and desirable pharmacokinetic properties (MMV253).
Key stages in the hit to lead pathway of MMV253. Initial replacement of ethylbenzene on M’1 with 2-methylpyridine resulted in lower hERG affinity and improved solubility. Substitution of the pyrrolidine in M’2 with an imidazole containing an amine spacer further improved solubility and greatly improved the potency. Addition of an N-methyl group and a cyclopropane moiety led to the optimized compound MMV253
When screened against numerous mutant resistant strains with various mechanisms of resistance, MMV253 showed no spontaneous reduction in potency which can be attributed to its novel MoA (PfATP4 inhibition, vide infra). Good in vitro-in vivo correlation (IVIVC) was shown with a predicted human half-life of \(\sim\) 36 h (which is long compared to another fast-killing drug, artemisinin, which has a human half-life of 1 hour).
As of late 2016, the pharmaceutical company Cadila Healthcare owns the license for the compound series and is now doing further lead development in order to progress the drug through preclinical trials [82].
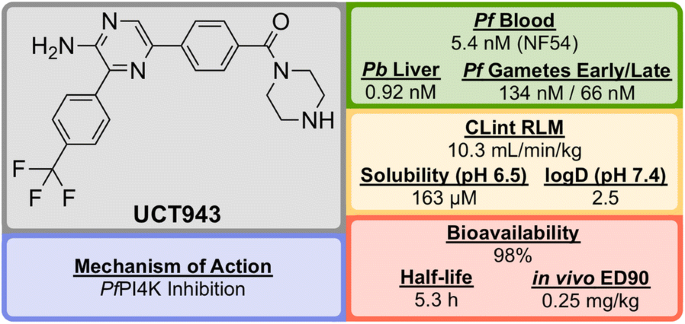
UCT943 (Fig. 10) was identified in 2016 by a team at the University of Cape Town, South Africa and is a key compound in a novel class of 2-aminopyrazine anti-malarials that has shown single dose curing ability in vivo and potential as a clinical candidate [83].
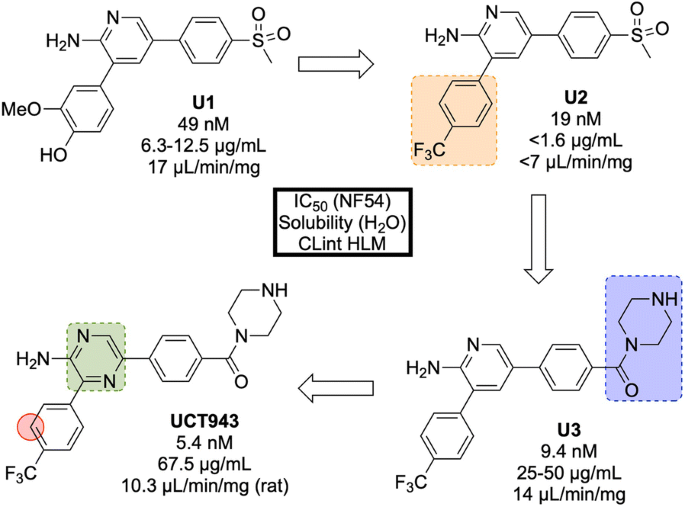
The original 3,5-diaryl-2-aminopyridine series was identified from a high-throughput screen of 36608 compounds from the commercially available SoftFocus kinase library [84]. The initial hit (U1, Fig. 11) showed promising in vitro activity against the drug-sensitive NF54 strain (IC\(_{50}\) = 49 nM) but suffered from poor solubility and high metabolic clearance. To address the poor measured in vivo stability, the labile hydroxy and methoxy groups were replaced by a single trifluoromethyl group (U2), but this change resulted in a significant loss of solubility. Significant improvements in solubility and potency were obtained by first replacing the mesyl group with a piperazine carboxamide group (U3) and subsequently introducing another nitrogen atom into the pyridine ring (UCT943) [85, 86].
Key stages in the hit to lead pathway of UCT943. Initial change the phenyl substituents with a single trifluoromethyl group led to greater in vivo stability. Introduction of piperazine amide instead of methylsulfonyl and a pyrazine instead of a pyridine led to the improved solubility and potency of the optimized compound. Surprisingly, introduction of a nitrogen in the red circle resulted in complete inactivity in vivo
In the P. berghei mouse model, UCT943 has shown the ability to cure malaria at doses of 4 \(\times\) 10 mg/kg and has an ED\(_{90}\) of 1 mg/kg. Interestingly, another closely related molecule (with a nitrogen instead of a carbon in the red circle) which was evaluated during the SAR study, displayed similar in vitro anti-malarial activity (IC\(_{50}\) = 9.1 nM) and solubility (198 \(\mu\)M) but showed a complete lack of in vivo activity with a < 40% reduction in parasitaemia using a comparable dosage.
UCT943 is potent across multiple parasite life stages of both P. falciparum and P. vivax. Its target is Plasmodium phosphatidylinositol-4-OH kinase (PfPI4K), which has also been implicated as the target for MMV048 (vide infra) [87]. UCT943 was in originally in place as a back-up to MMV048, however, due to preclinical toxicity, this candidate has been withdrawn.
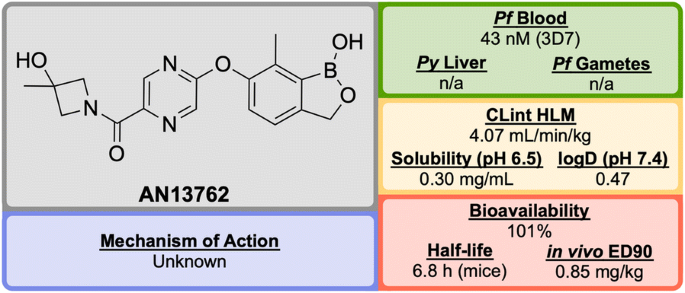
From a discovery process by Anacor Pharmaceuticals that began in 2010 with a novel class of benzoxaborole anti-malarial compounds [88], AN13762 (Fig. 12) emerged in 2017 as the lead compound, showing excellent activity in vitro and in vivo, multi-strain efficacy and the ability to perform as a rapid-acting drug [89].
By screening a library of boron-containing compounds (previously shown to have selective activity against fungi, bacteria, parasites and inflammation) in a whole cell assay against P. falciparum, the initial hit compound, AN3661 (A1, Fig. 13), was identified to have potent in vitro activity against the 3D7 strain (IC\(_{50}\) = 26 nM). Further SAR and optimization studies led to the development of A2 in which the alkylcarboxylic acid chain was moved and replaced by a substituted pyrazine ether. This compound showed greater potency but still suffered from high metabolic clearance [90]. Replacement of the ester group with an amide group (A3) led to improved metabolic stability and bioavailability, with a significant decrease in potency. Modification of the primary amide to a cyclic tertiary amide, and introduction of a methyl group on the benzoxaborole gave the lead compound AN13762 which possessed improved potency and metabolic stability [89].
AN13762 has been shown to be equally potent across a wide range of drug resistant strains. The drug has displayed similar in vivo clearance rates when compared to artesunate. There is no inherent genotoxicity (as shown in Ames assays and in vivo rat micronucleus studies), and no cytotoxicity at concentrations up to 100 μM in human cell lines [89].
The precise mechanism of action for AN13762 remains unknown, though initial MoA studies on hit compound AN3661 identified a potential target as the P. falciparum cleavage and polyadenylation specificity factor (PfCPSF3) [91]. AN13762 has proceeded into the preclinical phase, with first-in-human studies planned for 2019 [58].
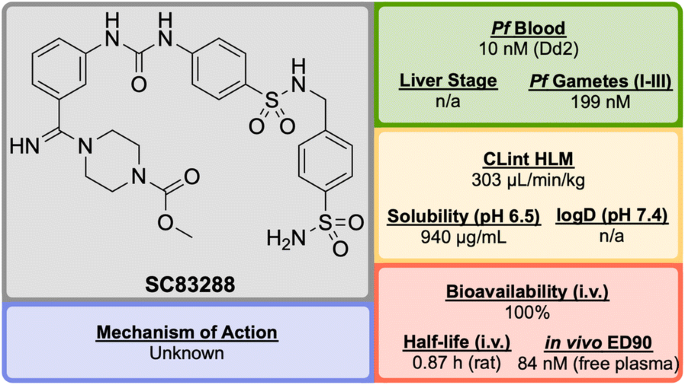
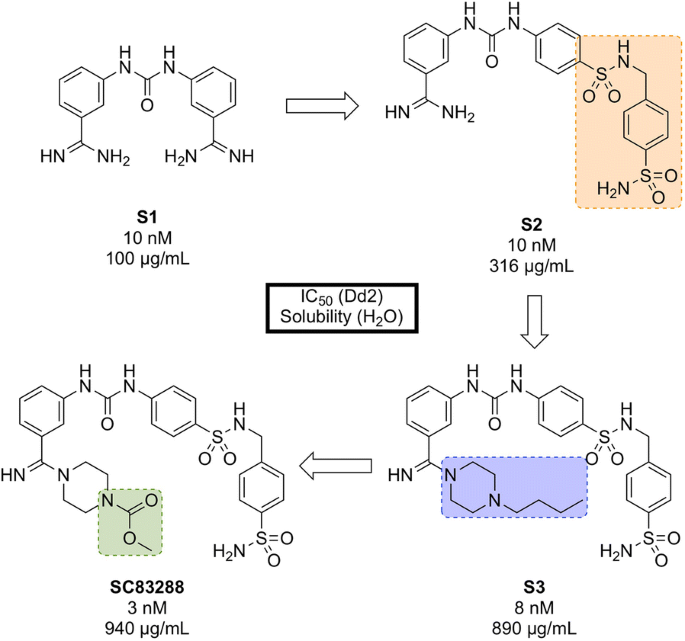
Developed in 2017 by a team at Heidelberg University, SC83288 (Fig. 14) is an amicarbalide derivative that possesses a novel chemotype for current anti-malarials, may have a potentially new MoA and has shown the ability to be a fast-acting drug for the intravenous treatment of severe malaria [92].
An in silico screen of a library of small molecule compounds for their ability to dock into P. falciparum lactate dehydrogenase led to the identification of amicarbalide (S1, Fig. 15), which was found to be highly potent (IC\(_{50}\) = 10 nM) against the Dd2 strain [93]. In order to overcome a potential DNA binding effect, an amidine group was replaced with a sulfonamide linker leading to S2 which possessed better solubility and improved metabolic stability. Further modification of the other amidine group with a substituted piperazine ring (S3) led to improved potency and water solubility, but the compound suffered from poor permeability. Ultimately, replacement of the butyl chain with an acetyl group led to the highly potent lead compound SC83288.
Key compounds in the discovery of SC83288. Initial modification of one amidino group with a sulfonamide linker (S2) resulted in improved solubility. Further modification of the remaining amidine group with substituted piperazine moieties ultimately led to the optimized compound with good solubility, permeability and high potency
SC83288 has been shown to be potent against a number of drug-resistant strains at IC\(_{50}\) values of < 20 nM and is also efficacious against early stage (I–III) gametocytes (IC\(_{50}\) = 199 nM) but not against late stage gametocytes (IV and V). It has an excellent safety profile, with no cytotoxicity, genotoxicity or hERG binding. In the Plasmodium vinckei rodent malaria model, SC83288 was able to fully cure the infection at a dose of 4 \(\times\) 20 mg/kg i.p. q.d. with no resurgence of infection. It is however, completely inactive against P. berghei.
While the exact MoA of SC83288 is unknown, the generation of resistant clones has identified PfATP6 as a possibly relevant target. However, it has been shown that SC83288 does not directly inhibit this target suggesting PfATP6 may have a less direct role in the mechanism of SC83288. PfMDR2 has been identified as another possible mechanism of resistance, facilitating the clearance of the drug from the parasite. SC83288 has been evaluated against artemisinins, showing no cross resistance and highlighting its potential as an alternative to artesunate for the treatment of severe malaria when combined with a slow-acting partner drug [94].
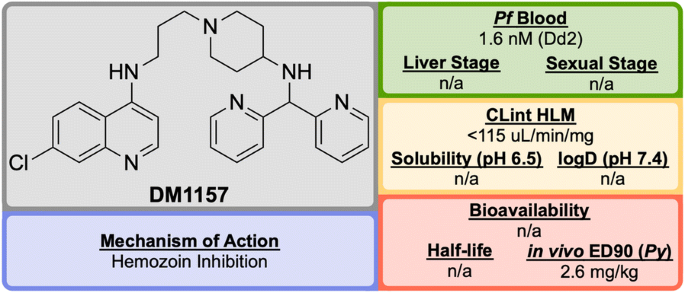
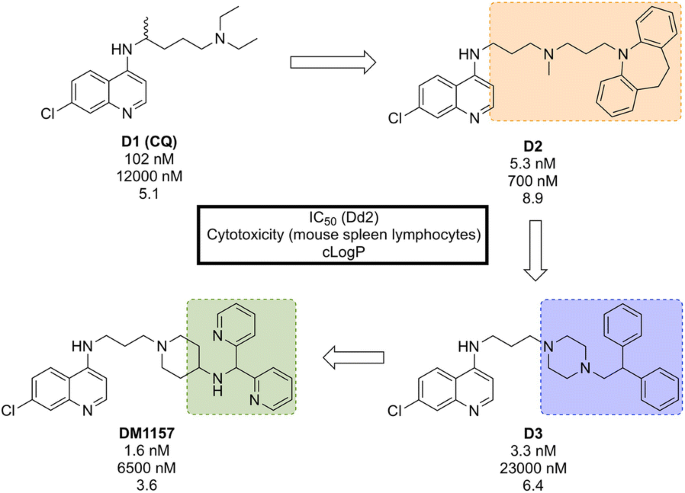
Discovered in 2010 by a team at Portland State University and further developed by DesignMedix, DM1157 (Fig. 16) is part of a class of compounds known as “reversed chloroquines” (RCQs), designed to overcome chloroquine-resistant and chloroquine-sensitive strains of the malaria parasite. The compound has been shown to be efficacious in vitro and in vivo [95].
CQ resistance is known to be linked to the P. falciparum chloroquine resistance transporter (PfCRT): mutations to this target facilitate the expulsion of CQ from the parasite. A class of molecules has been identified, so-called “reversal agents”, that can inhibit PfCRT, thus slowing the exportation of CQ from the parasite. By combining the chloroquinoline core of CQ (D1, Fig. 17) with the known reversal agent, imipramine, the first RCQ (D2) was designed, but this molecule suffered from poor bioavailability and metabolic stability [96]. Subsequent SAR studies resulted in the substitution of the imipramine motif with a 1-(2,2-diphenylethyl)piperazine moiety which led to a compound (D3) that was more stable to metabolic cleavage, but suffered from a high cLogP. In order to overcome this, the two phenyl groups were replaced with pyridines and the piperazine replaced with an aminopiperidine resulting in the lead compound, DM1157 that possessed a lower cLogP value (3.6) while still maintaining high potency against both CQ-resistant (Dd2 = 1.6 nM) and CQ sensitive strains (D6 = 0.9 nM) when compared to CQ (cLogP = 5.1, Dd2 = 102 nM, D6 = 6.9 nM).
Key compounds in the discovery of DM1157. Initial combination of the reversal agent, imipramine, with the CQ core resulted in the potent RCQ compound D2. Subsequent replacement of the reversal agent with 1-(2,2-diphenylethyl)piperazine (D3), and further modification with pyridine rings led to improved potency and cLogP values for the optimized compound
In a P. berghei rodent model, DM1157 showed good efficacy both orally and subcutaneously. Most notably, a > 99.9% reduction in parasitaemia was seen at an oral dose of 4 \(\times\) 30 mg/kg with 2/3 mice cured 30 days post infection. DM1157 has also been evaluated against P. falciparum and P. vivax multi-drug resistant field isolates in Indonesia and was found to be threefold more potent than CQ in both species [97].
CQ is known to bind to heme and inhibit \(\beta\)-haemozoin formation. DM1157 (and other RCQ compounds) have been shown also to act in this manner, but with much higher levels of inhibition of \(\beta\)-haemozoin both in vitro and in vivo. DM1157 is currently in Phase I trials to evaluate its safety and pharmacokinetics in humans (NCT03490162).
Translational (human volunteers)
Upon the completion of preclinical trials, the drug will have either passed or failed the required safety standards and pharmacokinetic profiling. For a compound that has passed these requirements, trials may then be conducted in human volunteers in order to show its efficacy as a potential treatment.
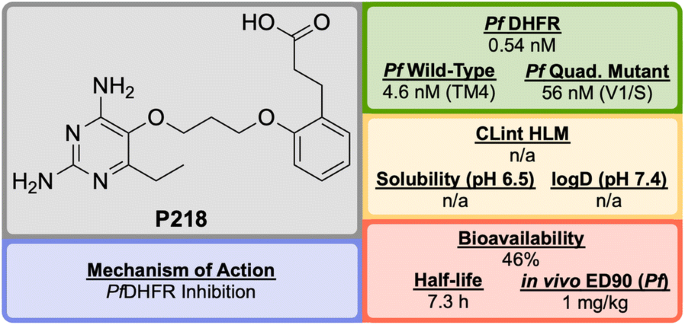
P218 (Fig. 18), discovered by BIOTEC Thailand in 2012, is an antifolate anti-malarial drug bearing resemblance to the 2,4-diaminopyrimidine core structure of PYR, and is highly selective for the P. falciparum dihydrofolate reductase (PfDHFR) [98].
Unlike the typical high-throughput screening that is used for the identification of hit compounds in medicinal chemistry, P218 was identified through careful examination of the cocrystal structures of known PfDHFR inhibitors and their substrates. The initial observation that 2,4-diaminopyrimidines acted as antagonists to folic acid led to the discovery and development of methotrexate (MTX) as an antitumor drug (Fig. 19). By examining the binding interactions with DHFR, the structure of P65 was identified. A total of over 200 compounds (not described in the original report) were designed and synthesized after further examination of potential interactions with amino acid residues, with the optimized structure of P218 being identified as the best compound.
The 2,4-diaminopyrimidine scaffold of P218 has been found to bind deep in the active site of PfDHFR in both wild-type and mutant strains. This, along with the hydrogen bonding interaction of the carboxylate group with an Arg residue at the opposite end of the active site results in tighter binding and a longer residence time when compared to PYR. Since P218 is contained almost entirely within the dihydrofolate binding site, the strength of the binding should be strong enough to overcome any amino acid mutations, thus minimising the chance of drug-resistant mutations to arise. The novel two-step mechanism of action for binding to PfDHFR (vide infra) allows P218 to overcome resistance that has emerged from the use of pyrimethamine. P218 has also shown high selectivity to the binding of malarial over human DHFR, which translates into reduced toxicity.
In vivo studies have shown P218 to be highly efficacious against P. falciparum and Plasmodium chabaudi in mice with ED\(_{90}\) values of 1 mg/kg and 0.75 mg/kg respectively. In the in vitro and in vivo potency assays that were run, P218 was found to be more potent than PYR in all cases.
Along with its high potency and good safety profile, P218 has the potential to be a replacement for PYR combination with CG in areas where PfDHFR resistance has emerged. P218 has currently completed Phase I trials (NCT02885506).
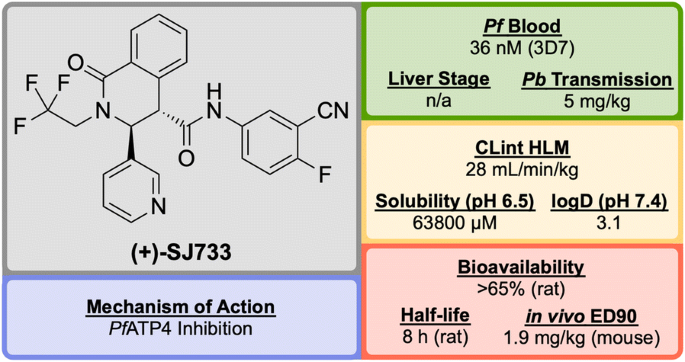
Discovered by a partnership between St Jude Children’s Research Hospital and Rutgers University in 2010, (+)-SJ733 (Fig. 20) is a novel tetrahydroisoquinolone carboxanilide that possesses excellent anti-malarial activity in vivo [99].
High-throughput phenotypic screening of > 300,000 compounds against the 3D7 strain of P. falciparum discovered a number of bioactive scaffold types, in which the hit compound (S′1, Fig. 21), belonging to the tetrahydroisoquinolone carboxanilide class, was found to have potent in vitro activity (EC\(_{50}\) = 53 nM). Metabolic studies using mouse liver microsomes identified the susceptibility of the methoxy group to demethylation. In order to overcome this issue, the aniline substituents were replaced with fluoro and cyano groups (S′2), which had an added effect of improving the potency more than twofold. The thiophene group was suspected to be a metabolic hot spot, which was addressed by its replacement with a pyridyl group (S′3) resulting also in improved solubility, while maintaining potency. The final metabolically labile group (isobutyl) was replaced with a trifluoromethyl moiety, further improving solubility and maintaining potency to give the lead compound (+)-SJ733. The (+)-(3S,4S) isomer was found to be significantly more potent (EC\(_{50}\) = 36 nM) than its (–)-(3R,4R) enantiomer (EC\(_{50}\) = 587 nM) [100].
Key stages in the hit to lead pathway of (+)-SJ733. Poor metabolic stability of the hit compound was addressed by replacement of the chloro and methoxy groups with cyano and fluoro groups respectively. Further in vivo stability and solubility improvements were made by changing the thiophene to a pyridine. Finally, the gem-dimethyl group was substituted with a trifluoromethyl group to eliminate possible metabolic oxidation
In the P. berghei mouse model, (+)-SJ733 was found able to cure malaria at doses of 4 \(\times\) 100 mg/kg and has an ED\(_{90}\) of 1.9 mg/kg. It has shown transmission blocking activity in infected mice with an ED\(_{50}\) of 5 mg/kg. It possesses a good safety profile with no cytotoxicity and was found to be more potent in vivo when compared to existing anti-malarials such as artesunate, chloroquine, and pyrimethamine [101].
The molecular target of (+)-SJ733 has been identified as the P-type Na\(^+\)–ATPase transporter (PfATP4, vide infra), which has been implicated as a target for a number of other structurally diverse compounds [102]. The compound is currently in the recruiting stage of first-in-human study trials (NCT02661373).
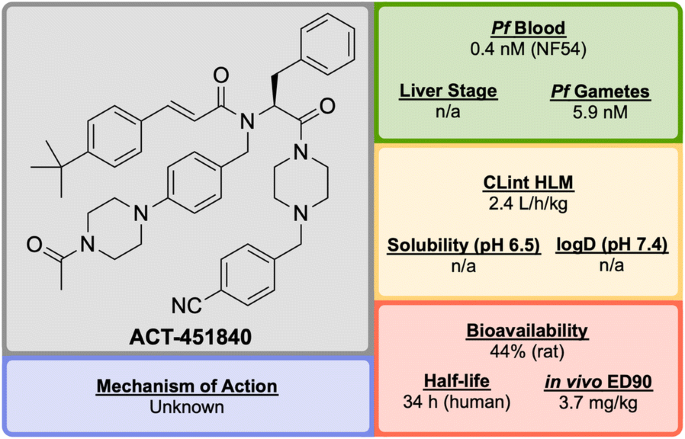
ACT-451840 (Fig. 22) is a phenylalanine-based compound that was developed in 2016 through a collaboration between Actelion Pharmaceuticals and the Swiss Tropical and Public Health Institute (STPHI). It has the potential to be a fast-acting drug with a long half-life and has shown efficacy against multiple stages of the P. falciparum parasite [103].
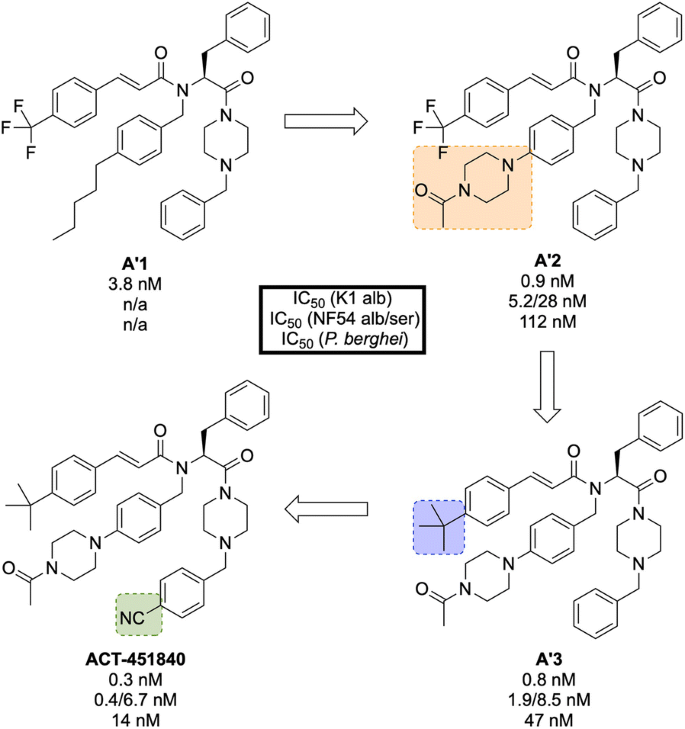
Initial erythrocyte-based phenotypic screening of \(\sim\) 5000 compounds identified A′1 (Fig. 23) as a highly potent compound against the chloroquine-resistant K1 strain of P. falciparum (IC\(_{50}\) = 3.8 nM). The SAR studies in this project were unique in that the anti-malarial activity was measured in parallel in two different media: 10% bovine serum albumin and 50% human serum, with the latter used to help identify any potential problems with protein binding at an early stage of the optimization. The stereogenic centre of the amino acid residue proved to be important for the activity, with the (S)-isomer showing more than tenfold higher activity compared to the non-natural (R)-isomer. Modification of the n-pentyl chain to an acylpiperazine group (A′2) resulted in an improvement in the physical and chemical properties of the compound. Replacement of the trifluoromethyl group with a tert-butyl group (A′3) led to improved anti-malarial activity, especially in the presence of human serum proteins. Final installation of a 4-cyano moiety on the southern phenyl ring gave the highly potent (IC\(_{50}\) = 0.4 nM) lead candidate ACT-451840.
Key stages in the hit to lead pathway of ACT-451840. Initial change of the n-pentyl group to an acylpiperazine (A′2) helped to improve the physicochemical properties. Subsequent introduction of a tert-butyl in place of the trifluoromethyl (A′3) and a cyano group on the southern phenyl ring resulted in the optimized compound
Interestingly, all compounds were found to be significantly less active against P. berghei than the human parasite. This is notable since most new anti-malarial drugs in development have shown similar potency against both rodent and human parasites. As a result, for in vivo studies it was crucial to use a humanized P. falciparum severe combined immunodeficiency (SCID) mouse model. In the P. berghei mouse model, ACT-451840 showed the ability to cure malaria at doses of 3 \(\times\) 300 mg/kg with an ED\(_{90}\) of 13 mg/kg. In the P. falciparum SCID mouse model it had an ED\(_{90}\) of 3.7 mg/kg. The importance of the delivery system for ACT-451840 was shown through in vivo experiments: a 60 mg dose in corn oil was as effective as a 100 mg dose in a mixture of Tween-EtOH/water = 10:90.
ACT-451840 has shown activity against multiple parasite life cycle stages of both P. falciparum and P. vivax [104]. The MoA is suspected to be novel but is currently unknown. ACT-451840 last completed first-in-human studies in 2014 (NCT02223871) [105] and is currently awaiting a decision to proceed.
Product development (patient exploratory)
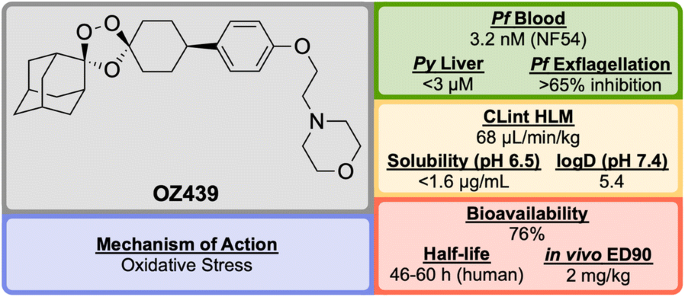
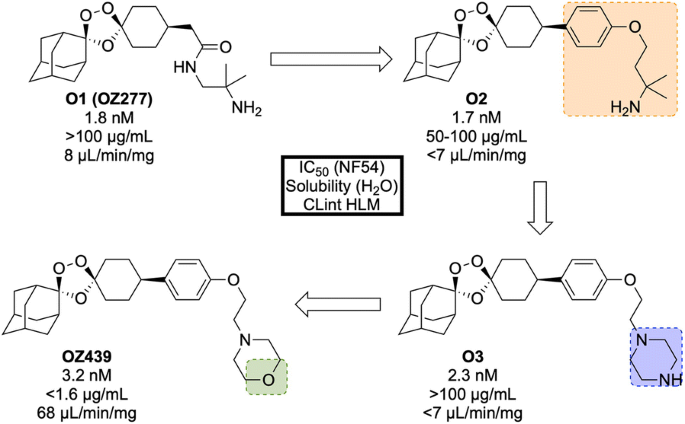
Discovered in 2011 by a partnership between Monash University, the University of Nebraska and the STPHI, OZ439 (Fig. 24) is a synthetic trioxolane that possesses fast-acting curative and transmission-blocking ability, and is active against artemisinin-resistant parasites [106].
The discovery of OZ439 (a.k.a. Artefenomel) stems from the lead optimization of the pre-existing trioxolane OZ277 (O1, Fig. 25, a.k.a. Arterolane), which was discovered in 2004 [107, 108]. As previous studies have shown that the adamantane-peroxide moiety is essential for anti-malarial activity, studies were focused on the eastern portion of the molecule [109,110,111]. Notably, analogues with variation in this area were found to have largely similar in vitro activities. In order to improve upon the original lead compound OZ277 (mean survival 11 days, 0 from 5 mice cured), replacement of the amide linker with a phenyl ether linker (O2) led to improved exposure and single-dose curative efficacy (mean survival > 30 days, 5 from 5 mice cured when applied in single dose of 30 mg/kg 1 day after infection). An attempt to further improve the exposure saw replacement of the alkylamine chain with a terminal piperazine unit (O3), however this led to a significant reduction in curative efficacy (mean survival 17 days, 0 from 5 mice cured). Encouragingly, using morpholine (OZ439) resulted in a mean survival of > 30 days, with 5 from 5 mice cured [112]. While OZ439 has shown excellent curative efficacy, no clear correlations were found between in vitro and in vivo activity or physiochemical properties and exposure. As a result, this new lead compound possess significantly lower solubility and slightly lower potency than OZ277.
Key stages in the hit to lead pathway of OZ439. Initial replacement of the amide linker with a phenyl ether linker resulted in improved exposure while maintaining potency (O2). The exposure was further improved by changing the alkylamine chain to a piperazine ring (O3). Final replacement of the piperazine ring with a morpholine unit led to the optimized compound OZ439, which possessed better curative efficacy in vivo
Unlike other peroxide-containing anti-malarials (e.g. artemisinin), OZ439 was found to be curative at a single dose of 20 mg/kg in the P. berghei mouse model and possessed prophylactic activity superior to mefloquine when a 30 mg/kg dose was applied 24 h prior to malaria infection. OZ439 also showed full anti-malarial protection when administered 96 h before infection at a dose of 100 mg/kg. Only minor signs of toxicity were observed in a rat model when five consecutive doses of 300 mg/kg were administered with 3 days interval. Conversely, O2 resulted in the death of 9 from 12 animals when used at the same dose [112]. OZ439 has shown a significantly longer half-life in humans (about 46–62 h) when compared to the hit compound OZ277 (3 h) [113,114,115].
Much like the current peroxide-containing anti-malarials, the precise MoA for OZ439 has yet to be discovered but it is believed that oxidative stress plays a major role [116, 117]. First-in-human results for OZ439 were published in 2013 [118] and since then the molecule has progressed into Phase IIb clinical trials with planned completion in 2019 (NCT02497612) [119].
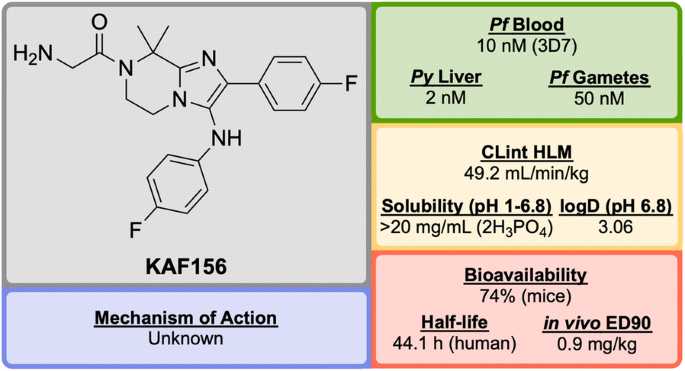
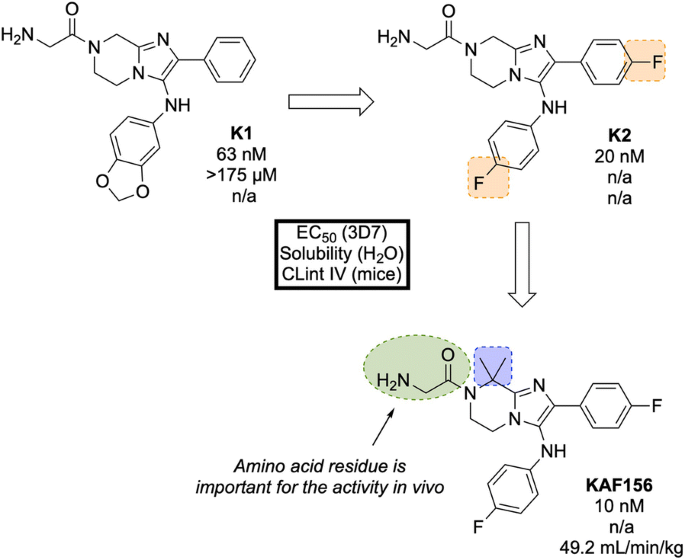
KAF156 (Fig. 26) was identified in 2008 by Novartis and The Scripps Research Institute and is part of the second-generation of imidazolopiperazine anti-malarials that potentially possesses a novel MoA and performs as a rapid-acting drug [120].
A high-throughput screen of 1.7 million compounds in a P. falciparum proliferation assay led to the identification of hit compound K1 (Fig. 27). In order to protect the metabolically vulnerable positions in the lead compound and to optimize the potency, the benzodioxole and phenyl fragments were replaced with 4-fluorobenzene groups (K2). Installation of a dimethyl group in the piperazine ring led to the twofold more potent compound KAF156 [121, 122]. Notably, removal of the glycine residue from the piperazine ring was shown to increase the in vitro potency further (EC\(_{50}\) = 5 nM), but this was accompanied by a lower parasitaemia reduction, indicating the importance of the amino acid side chain for in vivo efficacy [121].
In the causal prophylactic rodent malaria model, a single oral dose of 10 mg/kg administered 2 h before intravenous infection with P. berghei sporozoites was shown to be fully protective. KAF156 has also shown transmission blocking ability in the P. berghei model.
The MoA for KAF156 remains unknown. Through the culturing of resistant strains, mutations have been identified in three genes: P. falciparum Cyclic Amine Resistance Locus (PfCARL), UDP-galactose and Acetyl-CoA transporters [58, 123]. KAF156 is currently in Phase IIb clinical trials, administered in combination with Lumefantrine (NCT03167242).
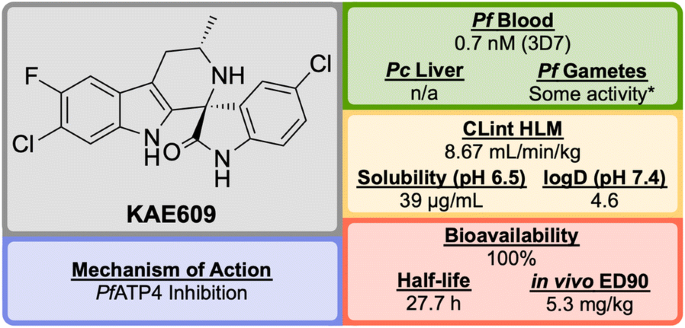
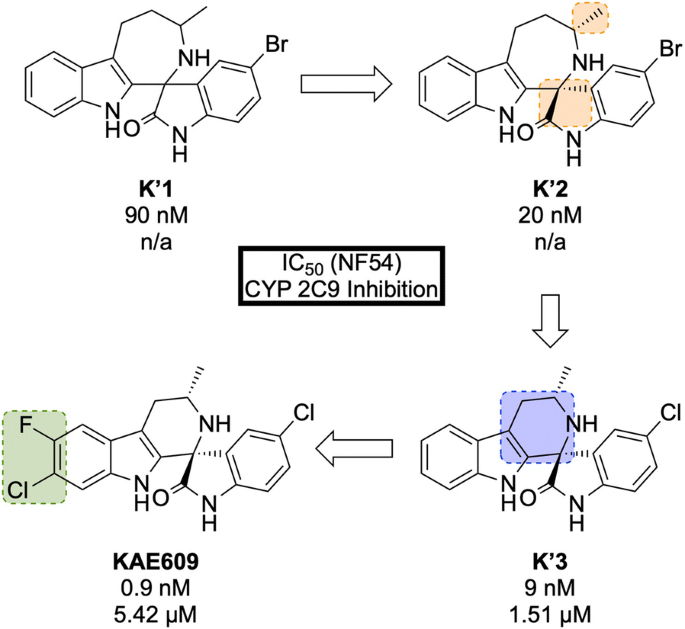
KAE609/Cipargamin/NITD609 (Fig. 28) was discovered by a partnership between Novartis, the STPHI and the Wellcome Trust [124, 125].
A high-throughput P. falciparum proliferation assay identified a racemic spiroazepineindole compound (K′1, Fig. 29) which possessed moderate potency against K1 and NF54 strains, as well as potent in vivo efficacy. Confirmation of the hit result by resynthesis of K′1 resulted in the isolation of a \(\sim\) 9:1 diastereomeric ratio favouring the (1R,3S) and (1S,3R) pair of enantiomers. Chiral separation of this major pair identified the (1R,3S) enantiomer K′2 as being > 250-fold more potent than the (1S,3R) enantiomer. Reduction of the ring size (K′3) facilitated a diastereoselective Pictet–Spengler reaction, which ultimately led to the production of highly potent spiroindolone KAE609.
KAE609 is equipotent against drug-resistant strains and was found to be as effective as artesunate against P. falciparum and P. vivax isolates [126]. It shows a good safety profile, with low cytotoxicity, cardiotoxicity and mutagenic activity, and is able to clear parasitaemia rapidly in adults with uncomplicated P. falciparum or P. vivax malaria at a dose of 30 mg/day for 3 days. KAE609 displays low clearance from the body, has a long half-life and excellent bioavailability.
KAE609 is one of the key novel compounds that has been found to act through inhibition of PfATP4 (vide infra). Along with a number of other structurally distinct compounds that are also thought to inhibit PfATP4 as their MoA, KAE609 has shown great promise as an new anti-malarial candidate and is currently in Phase IIb trials (NCT03334747).
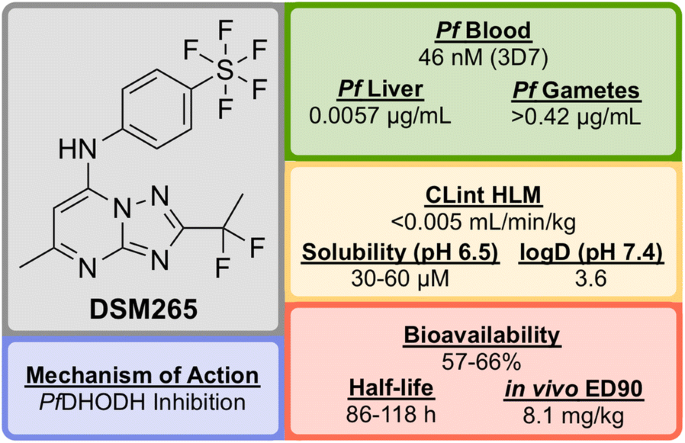
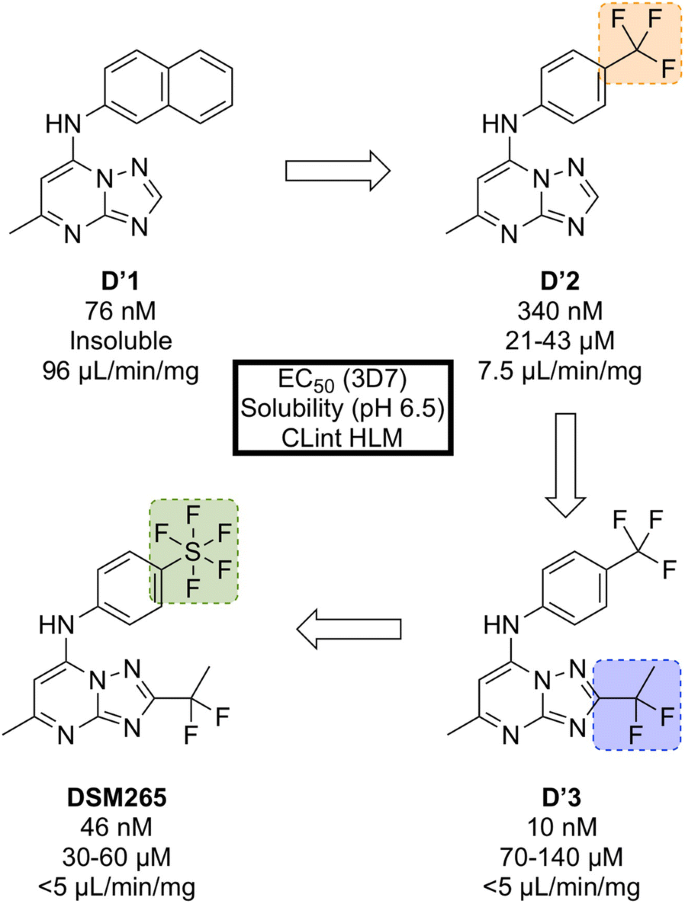
DSM265 (Fig. 30) was discovered through a collaboration between the University of Texas Southwestern, the University of Washington and Monash University [127].
Identified in a high-throughput screen of P. falciparum dihydroorotate dehydrogenase (PfDHODH)-based enzyme activity, the selective inhibitor D′1 (Fig. 31) was found. The compound showed high potency but was rapidly metabolized and was inactive in vivo. Substitution of the naphthyl ring with a trifluoromethylphenyl group led to a metabolically stable analogue (D′2). Examination of the bound crystal structures of D′1 and D′2 with PfDHODH identified key residue interactions which eventually led to the installation of a difluoroethyl group (D′3) which significantly improved the potency and solubility. Final modification of the trifluoromethyl group with a pentafluorosulfur group led to the optimized compound DSM265.
Key stages in the hit to lead pathway of DSM265. Replacement of the second phenyl ring in the naphthyl group with a trifluoromethyl group improved solubility. Addition of a 1,1-difluoroethyl group significantly increased the potency and final replacement of the trifluoromethyl group in D′2 with a pentafluorosulfur moiety led to the optimized compound DSM265
DSM265 has been shown to be a highly selective inhibitor of malarial DHODH and is potent against both blood and liver stages of P. falciparum and also drug-resistant parasite isolates. It has an excellent safety profile (provides therapeutic concentrations after 8 days of a single oral dose, tolerated in repeat-doses, non-mutagenic, inactive against human enzymes/receptors) and has a very low clearance rate and a long half-life in humans [128]. DSM265 has completed Phase IIa trials in Peru in patients with P. falciparum or P. vivax (NCT02123290) and also completed a controlled human malaria infection study in combination with OZ439 (NCT02389348).
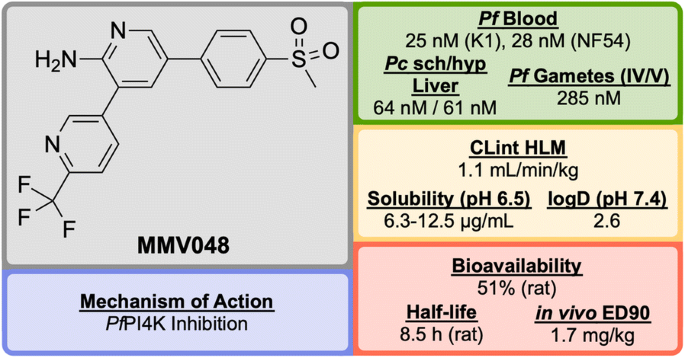
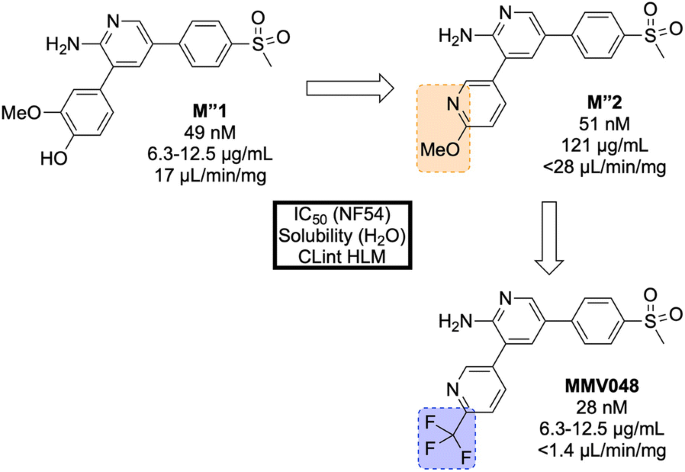
Identified in 2012 by a team at the University of Cape Town, South Africa in the same campaign as UCT943, MMV048 (Fig. 32) is another compound in the 3,5-diaryl-2-aminopyridine class that possesses good prophylactic activity against Plasmodium cynomolgi in vivo and has the potential to act as a transmission-blocking drug [84].
The initial hit (M″1, Fig. 33) showed potent in vitro activity against the NF54 (drug-sensitive) strain of P. falciparum (IC\(_{50}\) = 49 nM) but suffered from poor solubility and high metabolic clearance. The metabolically labile 3-methoxy-4-hydroxyphenyl moiety was replaced by a methoxypyridyl ring giving the more stable and equipotent compound M″2. Further SAR studies revealed that replacement of the methoxy group by a trifluoromethyl group led to the improved potency and stability of MMV048.
Key stages in the hit to lead pathway of MMV048. Initial replacement of the 3-methoxy-4-hydroxyphenyl moiety helped to improve in vivo stability and solubility. Further replacement of the methoxy group with a trifluoromethyl group improved potency and metabolic stability leading to the optimized compound
MMV048 has shown 99.3% reduction in parasitaemia in the P. berghei mouse model at a single dose of 30 mg/kg with no signs of parasites after 30 days (ED\(_{90}\) = 1.7 mg/kg). This highlights the potential of MMV048 to act as a single dose treatment.
The target of MMV048 is PfPI4K, which was recently revealed as a new MoA for anti-malarial drugs (vide infra) [87]. MMV048 is currently in Phase IIa clinical trials in Ethiopia [58].
Modes of action
The continual emergence of drug resistant Plasmodium strains means that developing new drugs with novel MoAs is important [129]. Below, are summarized some newer MoAs that are currently being pursued and which are exemplified by the compounds described above.
Translational elongation factor 2 (PfeEF2) inhibitor
The P. falciparum translational elongation factor 2 (PfeEF2) is one of the essential factors for eukaryotic protein synthesis, catalysing the translocation of tRNA and mRNA [130]. The overall efficacy of drugs that target this elongation factor may be increased due to PfeEF2 being expressed in multiple stages of the parasite life-cycle [78].
M5717 has been shown to inhibit PfeEF2 as its MoA, but a binding pocket for M5717 could not be elucidated from the modelling studies [78]. This MoA was found by culturing blood stage parasites with five times the EC\(_{50}\) of M5717, leading to resistance in the 3D7, 7G8 and Dd2 strains. Through whole-genome sequencing of these resistance lines, a common mutation was found which identified PfeEF2 as the target.
P-type Na\(^+\)–ATPase inhibitor (PfATP4) inhibitor
The malaria parasite must maintain a low intracellular Na\(^+\) concentration to survive, especially in the presence of the high concentration of extracellular sodium ions. In this case, the parasite’s influx of Na\(^+\) is regulated by using a P-type ATPase transporter (PfATP4) that shuttles sodium ions out of the cell. Inhibition of this transporter results in a build up of Na\(^+\) inside the parasite, ultimately leading to cell death [102].
A number of structurally diverse compounds (including (+)-SJ733 and KAE609) are thought to target PfATP4 as their MoA again suggested by the development of resistant mutants and sequencing [124]. The Kirk group have developed a fluorescence assay for this MoA [131], which has been used by the OSM project to implicate PfATP4 as a MoA for the Series 4 triazolopyrazines [132]. Of note, however, is that this MoA is suggested for a very broad range of chemotypes [133, 134], and there is no direct evidence for binding of these compounds to PfATP4, the structure of which remains unsolved.
V-type H\(^+\)–ATPase inhibitor
At the same time that the parasite is regulating its Na\(^+\) concentration through the above mechanism, it also imports H\(^+\) through the same pathway. To regulate this increasing H\(^+\) concentration and maintain an intracellular pH of \(\sim\) 7.3, the parasite uses a complementary V-type ATPase transporter to efflux H\(^+\) [135].
MMV253 has been shown to inhibit the V-type H\(^+\) ATPase as its MoA through mutant selection and whole-genome sequencing [81].
Phosphatidylinositol 4-kinase (PfPI4K) inhibitor
Phosphatidylinositol 4-kinase (PI4K) is a eukaryotic enzyme that phosphorylates lipids, allowing them to regulate intracellular signalling and trafficking [87]. Inhibition of the ATP-binding pocket of PI4K leads to disruption of the intracellular distribution of PI4-phosphate (PI4P), which in turn results in decreased late-stage parasite development.
By culturing resistant lines and identifying the genomic mutations, two compounds (UCT943 and MMV048) have been found to inhibit the PfPI4K enzyme [87].
Dihydroorotate dehydrogenase (PfDHODH) inhibitor
To be able to replicate in the human erythrocyte, the Plasmodium parasite requires pyrimidines, which are essential metabolites in all cells. As the parasite is unable to use endogenous pyrimidines, it must synthesize them de novo. A key step in the biosynthesis of pyrimidines is the oxidation of dihydroorotate to produce orotate, a reaction that is catalysed by the enzyme dihydroorotate dehydrogenase (DHODH). By inhibiting this enzyme, the malaria parasite can no longer obtain the required metabolites to survive, and is killed [136].
The P. falciparum D10 strain (chloroquine sensitive) has been known to be less susceptible to bc1 complex inhibitors and PfDHODH inhibitors. Addition of proguanil to this strain is known to restore the sensitivity to bc1 complex inhibitors but not to PfDHODH inhibitors. This cell line was found to be resistant to DSM265, regardless of whether proguanil was present or not, which identifies inhibition of PfDHODH as its MoA [127, 137].
Dihydrofolate reductase (PfDHFR) inhibitor
Similar to the above case, the malaria parasite also requires folates in order to maintain their high rate of replication. The parasite is able to scavenge folates or synthesize them de novo. Dihydrofolate reductase (DHFR) is an enzyme that catalyses a step required for the recycling of folates, which in turn are used in the synthesis of thymidylate, purines and methionine [138].
PfDHFR is a known target of a number of well known antifolate anti-malarial drugs including cycloguanil and pyrimethamine. Through examinations of the key interactions in the cocrystal structure of known inhibitors with the enzyme, P218 was designed as a potent inhibitor [98].
Conclusions
Although the rate of malaria related deaths has declined over the past few years, the progress is beginning to slow. With the recent emergence of resistance to current front-line artemisinin-based combination therapy, the need for the discovery of new anti-malarials that can act through novel mechanisms of action has been pushed firmly to the top of the development agenda.
Over the past few years, high-throughput screens have identified a number of novel chemotypes that have since been developed into highly promising anti-malarial candidates. Crucially, many of these compounds have demonstrated novel MoAs which are essential if future drugs are to succeed. This is wonderful progress, and testament to the hard work of the groups involved.
The discovery of these novel MoAs will pave the way for the development of future anti-malarials. The exploration of further novel MoAs has become a possibility through the use of in vitro evolution and whole-genome analysis (IVIEWGA), which uses genome-base target discovery methods on compounds identified from the more common phenotypic screens [139]. In all such future development, creativity and ingenuity in the hit to lead campaigns will continue to be needed if people are to remain able to combat this formidable disease.
The pace of research progress is high, meaning updates to reviews such as this will always be needed (Additional file 3). It is proposed that derivatives of this open access review, combined with data in relevant databases such as the one currently in development by the Guide to Pharmacology [140], could aim to serve as more “living” sources of information for compounds in development and their potential targets.
Abbreviations
- ACT:
-
artemisinin-based combination therapy
- CG:
-
cycloguanil
- CLint :
-
intrinsic clearance
- CQ:
-
chloroquine
- DDU:
-
Drug Discovery Unit
- EC50 :
-
half maximal effective concentration
- ED90 :
-
90% effective dose
- GSK:
-
GlaxoSmithKline
- hERG:
-
human ether-à-go-go-related gene
- HLM:
-
human liver microsome
- IC50 :
-
half maximal inhibitory concentration
- i.p.:
-
intraperitoneally
- IVIEWGA:
-
in vitro evolution and whole-genome analysis
- IVIVC:
-
in vitro-in vivo correlation
- MLEM:
-
Model List of Essential Medicines
- MLM:
-
mouse liver microsome
- MMV:
-
Medicines for Malaria Venture
- MoA:
-
mode/mechanism of action
- mRNA:
-
messenger ribonucleic acid
- MTX:
-
methotrexate
- OSM:
-
Open Source Malaria
- P. :
-
Plasmodium
- p.o. :
-
(per os) orally
- Pb :
-
Plasmodium berghei
- Pc :
-
Plasmodium cynomolgi
- Pf :
-
Plasmodium falciparum
- Pf ATP4:
-
Plasmodium falciparum ATPase transporter
- Pf CARL:
-
Plasmodium falciparum cyclic amine resistance locus
- Pf CPSF3:
-
Plasmodium falciparum cleavage and polyadenylation specificity factor
- Pf DHFR:
-
Plasmodium falciparum dihydrofolate reductase
- Pf DHODH:
-
Plasmodium falciparum dihydroorotate dehydrogenase
- Pf eEF2:
-
Plasmodium falciparum translational elongation factor 2
- Pf PI3K:
-
Plasmodium falciparum phosphatidylinositol-3-kinase
- Pf PI4K:
-
Plasmodium falciparum phosphatidylinositol-4-OH kinase
- Py :
-
Plasmodium yoelli
- PYR:
-
pyrimethamine
- q.d. :
-
(quaque die) one a day
- RCQ(s):
-
reversed chloroquine(s)
- SAR:
-
structure activity relationship
- SCID:
-
severe combined immunodeficiency
- STPHI:
-
Swiss Tropical and Public Health Institute
- TAP:
-
triaminopyrimidine
- TQ:
-
tafenoquine
- tRNA:
-
transfer ribonucleic acid
- WHO:
-
World Health Organization
References
World Malaria Report 2018. https://www.who.int/malaria/publications/world-malaria-report-2018/en/. Accessed 27 Nov 2018.
Cheney C. Fight against malaria stalling and could reverse, warns 2017 World Malaria Report. http://theconversation.com/global-malaria-report-reveals-africas-hits-and-misses-heres-what-to-do-88577. Accessed 24 Mar 2018.
Mwangi T. Global malaria report reveals Africa’s hits and missed: here’s what to do. https://www.devex.com/news/fight-against-malaria-stalling-and-could-reverse-warns-2017-world-malaria-report-91636. Accessed 24 Mar 2018.
Shanks GD, Edstein MD, Jacobus D. Evolution from double to triple-antimalarial drug combinations. Trans R Soc Trop Med Hyg. 2014;109:182–8.
Mishra M, Mishra VK, Kashaw V, Iyer AK, Kashaw SK. Comprehensive review on various strategies for antimalarial drug discovery. Eur J Med Chem. 2017;125:1300–20.
Phillips MA, Burrows JN, Manyando C, van Huijsduijnen RH, Voorhis WCV, Wells TNC. Malaria. Nat Rev Dis Primers. 2017;3:17050.
Okombo J, Chibale K. Recent updates in the discovery and development of novel antimalarial drug candidates. MedChemComm. 2018;9:437–53.
Ashley EA, Phyo AP. Drugs in development for malaria. Drugs. 2018;78:861–79.
Medicines for Malaria Venture. https://www.mmv.org/. Accessed 24 Mar 2018.
Williamson AE, Ylioja PM, Robertson MN, Antonova-Koch Y, Avery V, Baell JB, et al. Open source drug discovery: highly potent antimalarial compounds derived from the Tres Cantos arylpyrroles. ACS Cent Sci. 2016;2:687–701.
Leong FJ, Li R, Jain JP, Lefèvre G, Magnusson B, Diagana TT, et al. A first-in-human randomized, double-blind, placebo-controlled, single- and multiple-ascending oral dose study of novel antimalarial spiroindolone KAE609 (Cipargamin) to assess its safety, tolerability, and pharmacokinetics in healthy adult volunteers. Antimicrob Agents Chemother. 2014;58:6209–14.
Achan J, Talisuna AO, Erhart A, Yeka A, Tibenderana JK, Baliraine FN, et al. Quinine, an old anti-malarial drug in a modern world: role in the treatment of malaria. Malar J. 2011;10:144.
Bunnag D, Karbwang J, Na-Bangchang K, Thanavibul A, Chittamas S, Harinasuta T. Quinine-tetracycline for multidrug resistant falciparum malaria. Southeast Asian J Trop Med Public Health. 1996;27:15–8.
Model List of Essential Medicines. http://www.who.int/medicines/publications/essentialmedicines/en/. Accessed 24 Mar 2018.
Green R. A report on fifty cases of malaria treated with Atebrin. A new synthetic drug. Lancet. 1932;219:826–9.
Guttman P, Ehrlich P. Ueber die wirkung des methylenblau bei malaria. Berl Klin Wochenschr. 1891;28:953–6.
Schirmer RH, Coulibaly B, Stich A, Scheiwein M, Merkle H, Eubel J, et al. Methylene blue as an antimalarial agent. Redox Rep. 2003;8:272–5.
Lu G, Nagbanshi M, Goldau N, Jorge MM, Meissner P, Jahn A, et al. Efficacy and safety of methylene blue in the treatment of malaria: a systematic review. BMC Med. 2018;16:59.
Weina PJ. From atabrine in World War II to mefloquine in Somalia: the role of education in preventive medicine. Mil Med. 1998;163:635–9.
Loeb F. Activity of a new antimalarial agent, chloroquine (SN 7618). JAMA. 1946;130:1069–70.
Mushtaque M. Reemergence of chloroquine (CQ) analogs as multi-targeting antimalarial agents: a review. Eur J Med Chem. 2015;90:280–95.
Trenholme C, Williams R, Desjardins R, Frischer H, Carson P, Rieckmann K, et al. Mefloquine (WR 142,490) in the treatment of human malaria. Science. 1975;190:792–4.
Brasseur P, Druilhe P, Kouamouo J, Brandicourt O, Danis M, Moyou SR. High level of sensitivity to chloroquine of 72 Plasmodium falciparum isolates from southern Cameroon in January 1985. Am J Trop Med Hyg. 1986;35:711–6.
Foley M, Tilley L. Quinoline antimalarials: mechanisms of action and resistance. Int J Parasitol. 1997;27:231–40.
Nevin RL, Croft AM. Psychiatric effects of malaria and anti-malarial drugs: historical and modern perspectives. Malar J. 2016;15:332.
Cosgriff TM, Desjardins RE, Pamplin CL, Canfield CJ, Doberstyn EB, Boudreau EF. Evaluation of the antimalarial activity of the phenanthrenemethanol halofantrine (WR 171,669)*. Am J Trop Med Hyg. 1982;31:1075–9.
Croft AM. A lesson learnt: the rise and fall of Lariam and Halfan. J R Soc Med. 2007;100:170–4.
Qinghaosu Antimalaria Coordinating Research Group. Antimalarial studies on Qinghaosu. Chin Med J (Engl ). 1979;92:811–6.
The Nobel Prize in Physiology or Medicine 2015. https://www.nobelprize.org/nobel_prizes/medicine/laureates/2015/. Accessed 24 Mar 2018.
Eastman RT, Fidock DA. Artemisinin-based combination therapies: a vital tool in efforts to eliminate malaria. Nat Rev Microbiol. 2009;7:864–74.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin-resistant aalaria in western Cambodia. N Engl J Med. 2008;359:2619–20.
Amato R, Pearson RD, Almagro-Garcia J, Amaratunga C, Lim P, Suon S, et al. Origins of the current outbreak of multidrug-resistant malaria in southeast Asia: a retrospective genetic study. Lancet Infect Dis. 2018;18:337–45.
O’Neill PM, Barton VE, Ward SA. The molecular mechanism of action of artemisinin—the debate continues. Molecules. 2010;15:1705–21.
Wang J, Zhang CJ, Chia WN, Loh CCY, Li Z, Lee YM, et al. Haem-activated promiscuous targeting of artemisinin in Plasmodium falciparum. Nat Commun. 2015;6:10111.
Tilley L, Straimer J, Gnädig NF, Ralph SA, Fidock DA. Artemisinin action and resistance in Plasmodium falciparum. Trends Parasitol. 2016;32:682–96.
Shandilya A, Chacko S, Jayaram B, Ghosh I. A plausible mechanism for the antimalarial activity of artemisinin: a computational approach. Sci Rep. 2013;3:2513.
Mok S, Ashley EA, Ferreira PE, Zhu L, Lin Z, Yeo T, et al. Population transcriptomics of human malaria parasites reveals the mechanism of artemisinin resistance. Science. 2014;347:431–5.
Mbengue A, Bhattacharjee S, Pandharkar T, Liu H, Estiu G, Stahelin RV, et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature. 2015;520:683–7.
Berliner RW, Earle DP, Taggart JV, Zubrod CG, Welch WJ, Conan NJ, et al. Studies on the chemotheraphy of the human malarias. VI. The physiological disposition, antimalarial activity, and toxicity of several derivatives of 4-aminoquinoline. J Clin Invest. 1948;27:98–107.
Bompart F, Kiechel JR, Sebbag R, Pecoul B. Innovative public-private partnerships to maximize the delivery of anti-malarial medicines: lessons learned from the ASAQ Winthrop experience. Malar J. 2011;10:143.
Combrinck JM, Mabotha TE, Ncokazi KK, Ambele MA, Taylor D, Smith PJ, et al. Insights into the role of heme in the mechanism of action of antimalarials. ACS Chem Biol. 2012;8:133–7.
Chen L, Qu FY, Zhou YC. Field observations on the antimalarial piperaquine. Chin Med J (Engl ). 1982;95:281–6.
Vennerstrom JL, Ellis WY, Ager AL, Andersen SL, Gerena L, Milhous WK. Bisquinolines. 1. N,N-Bis(7-chloroquinolin-4-yl)alkanediamines with potential against chloroquine-resistant malaria. J Med Chem. 1992;35:2129–34.
Cui L, zhuan Su X. Discovery, mechanisms of action and combination therapy of artemisinin. Expert Rev Anti Infect Ther. 2009;7:999–1013.
Curd FHS, Davey DG, Rose FL. Studies on synthetic antimalarial drugs. Ann Trop Med Parasitol. 1945;39:208–16.
Hudson AT, Randall AW. Naphthoquinone derivatives. US5053432A; 1991.
Fry M, Pudney M. Site of action of the antimalarial hydroxynaphthoquinone, 2-[trans-4-(4’-chlorophenyl)cyclohexyl]-3-hydroxy-1,4-naphthoquinone (566C80). Biochem Pharmacol. 1992;43:1545–53.
Srivastava IK, Vaidya AB. A mechanism for the synergistic antimalarial action of atovaquone and proguanil. Antimicrob Agents Chemother. 1999;43:1334–9.
Russell PB, Hitchings GH. 2,4-Diaminopyrimidines as antimalarials. III. 5-Aryl derivatives. J Am Chem Soc. 1951;73:3763–70.
The Nobel Prize in Physiology or Medicine 1988. https://www.nobelprize.org/nobel_prizes/medicine/laureates/2015/. Accessed 19 June 2018.
Laing AB. Treatment of acute falciparum malaria with sulphorthodimethoxine (fansil). Br Med J. 1965;1:905–7.
Lumb V, Das MK, Singh N, Dev V, Khan W, Sharma YD. Multiple origins of Plasmodium falciparum dihydropteroate synthetase mutant alleles associated with sulfadoxine resistance in India. Antimicrob Agents Chemother. 2011;55:2813–7.
Zheng XY, Xia Y, Gao FH, Chen C. Synthesis of 7351, a new antimalarial drug. Yao Xue Xue Bao. 1979;14:736–7.
Chang C, Lin-Hua T, Jantanavivat C. Studies on a new antimalarial compound: pyronaridine. Trans R Soc Trop Med Hyg. 1992;86:7–10.
Croft SL, Duparc S, Arbe-Barnes SJ, Craft J, Shin CS, Fleckenstein L, et al. Review of pyronaridine anti-malarial properties and product characteristics. Malar J. 2012;11:270.
US FDA approves Krintafel (tafenoquine) for the radical cure of P. vivax malaria 2018. https://www.mmv.org/newsroom/press-releases/us-fda-approves-krintafel-tafenoquine-radical-cure-p-vivax-malaria. Accessed 25 Sept 2018.
Ebstie YA, Abay SM, Tadesse WT, Ejigu DA. Tafenoquine and its potential in the treatment and relapse prevention of Plasmodium vivax malaria: the evidence to date. Drug Des Devel Ther. 2016;10:2387–99.
MMV-Supported Projects. https://www.mmv.org/research-development/mmv-supported-projects. Accessed 14 Jun 2018.
Wells TNC, Gutteridge WE. Neglected diseases and drug discovery. Palmer MJ, Wells TNC, editors. RSC; 2012.
Burrows JN, Duparc S, Gutteridge WE, van Huijsduijnen RH, Kaszubska W, Macintyre F, et al. New developments in anti-malarial target candidate and product profiles. Malar J. 2017;16:26.
McChesney JD, Nanayakkara DNP, Bartlett M, Ager AL. Preparation of 8-(aminoalkylamino)quinolines as parasiticides. WO 9736590 A1; 1997.
Tekwani BL, Walker LA. 8-Aminoquinolines: future role as antiprotozoal drugs. Curr Opin Infect Dis. 2006;19:623–31.
Nanayakkara NPD, Ager AL, Bartlett MS, Yardley V, Croft SL, Khan IA, et al. Antiparasitic activities and toxicities of individual enantiomers of the 8-aminoquinoline 8-[(4-amino-1-methylbutyl)amino]-6-methoxy-4-methyl-5-[3,4-dichlorophenoxy]quinoline succinate. Antimicrob Agents Chemother. 2008;52:2130–7.
Marcsisin SR, Sousa JC, Reichard GA, Caridha D, Zeng Q, Roncal N, et al. Tafenoquine and NPC-1161B require CYP 2D metabolism for anti-malarial activity: implications for the 8-aminoquinoline class of anti-malarial compounds. Malar J. 2014;13:2.
Powles MA, Allocco J, Yeung L, Nare B, Liberator P, Schmatz D. MK-4815, a potential new oral agent for treatment of malaria. Antimicrob Agents Chemother. 2012;56:2414–9.
Singh C, Puri SK. Substituted 1,2,4-trioxanes as antimalarial agents and a process of producing the substituted 1,2,4-trioxanes. US6316493 B1; 2001.
Shafiq N, Rajagopalan S, Kushwaha HN, Mittal N, Chandurkar N, Bhalla A, et al. Single ascending dose safety and pharmacokinetics of CDRI-97/78: first-in-human study of a novel antimalarial drug. Malar Res Treat. 2014;2014:372521.
O’Neill PM, Shone AE, Stanford D, Nixon G, Asadollahy E, Park BK, et al. Synthesis, antimalarial activity, and preclinical pharmacology of a novel series of 4’-fluoro and 4’-chloro analogues of amodiaquine. Identification of a suitable “back-up” compound for N-tert-butyl isoquine. J Med Chem. 2009;52:1828–44.
Bora S, Chetia D, Prakash A. Synthesis and antimalarial activity evaluation of some isoquine analogues. Med Chem Res. 2010;20:1632–7.
O’Neill PM, Park BK, Shone AE, Maggs JL, Roberts P, Stocks PA, et al. Candidate selection and preclinical evaluation of N-tert-butyl isoquine (GSK369796), an affordable and effective 4-aminoquinoline antimalarial for the 21st century. J Med Chem. 2009;52:1408–15.
Haynes RK, Fugmann B, Stetter J, Rieckmann K, Heilmann HD, Chan HW, et al. Artemisone—a highly active antimalarial drug of the artemisinin class. Angew Chem Int Ed. 2006;45:2082–8.
Nicolas O, Margout D, Taudon N, Wein S, Calas M, Vial HJ, et al. Pharmacological properties of a new antimalarial bisthiazolium salt, T3, and a corresponding prodrug, TE3. Antimicrob Agents Chemother. 2005;49:3631–9.
Drake NL, Creech HJ, Garman JA, Haywood ST, Peck RM, van Hook JO, et al. Synthetic antimalarials. The preparation of certain 4-aminoquinolines\(^{1}\). J Am Chem Soc. 1946;68:1208–13.
Ramanathan-Girish S, Catz P, Creek MR, Wu B, Thomas D, Krogstad DJ, et al. Pharmacokinetics of the antimalarial drug, AQ-13, in rats and cynomolgus macaques. Int J Toxicol. 2004;23:179–89.
Sáenz FE, Mutka T, Udenze K, Oduola AMJ, Kyle DE. Novel 4-aminoquinoline analogs highly active against the blood and sexual stages of Plasmodium in vivo and in vitro. Antimicrob Agents Chemother. 2012;56:4685–92.
Mzayek F, Deng H, Mather FJ, Wasilevich EC, Liu H, Hadi CM, et al. Randomized dose-ranging controlled trial of AQ-13, a candidate antimalarial, and chloroquine in healthy volunteers. PLoS Clin Trials. 2007;2:e6.
Koita OA, Sangaré L, Miller HD, Sissako A, Coulibaly M, Thompson TA, et al. AQ-13, an investigational antimalarial, versus artemether plus lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria: a randomised, phase 2, non-inferiority clinical trial. Lancet Infect Dis. 2017;17:1266–75.
Baragaña B, Hallyburton I, Lee MCS, Norcross NR, Grimaldi R, Otto TD, et al. A novel multiple-stage antimalarial agent that inhibits protein synthesis. Nature. 2015;522:315–20.
Baragaña B, Norcross NR, Wilson C, Porzelle A, Hallyburton I, Grimaldi R, et al. Discovery of a quinoline-4-carboxamide derivative with a novel mechanism of action, multistage antimalarial activity, and potent in vivo efficacy. J Med Chem. 2016;59:9672–85.
Burrows JN, van Huijsduijnen RH, Möhrle JJ, Oeuvray C, Wells TN. Designing the next generation of medicines for malaria control and eradication. Malar J. 2013;12:187.
Hameed PS, Solapure S, Patil V, Henrich PP, Magistrado PA, Bharath S, et al. Triaminopyrimidine is a fast-killing and long-acting antimalarial clinical candidate. Nat Commun. 2015;6:6715.
MMV and Zydus join forces to develop new antimalarial 2017. https://www.mmv.org/newsroom/press-releases/mmv-and-zydus-join-forces-develop-new-antimalarial. Accessed 17 June 2018.
Manach CL, Nchinda AT, Paquet T, Cabrera DG, Younis Y, Han Z, et al. Identification of a potential antimalarial drug candidate from a series of 2-aminopyrazines by optimization of aqueous solubility and potency across the parasite life cycle. J Med Chem. 2016;59:9890–905.
Younis Y, Douelle F, Feng TS, Cabrera DG, Manach CL, Nchinda AT, et al. 3,5-Diaryl-2-aminopyridines as a novel class of orally active antimalarials demonstrating single dose cure in mice and clinical candidate potential. J Med Chem. 2012;55:3479–87.
Cabrera DG, Douelle F, Younis Y, Feng TS, Manach CL, Nchinda AT, et al. Structure-activity relationship studies of orally active antimalarial 3,5-substituted 2-aminopyridines. J Med Chem. 2012;55:11022–30.
Younis Y, Douelle F, Cabrera DG, Manach CL, Nchinda AT, Paquet T, et al. Structure-activity-relationship studies around the 2-amino group and pyridine core of antimalarial 3,5-diarylaminopyridines lead to a novel series of pyrazine analogues with oral in vivo activity. J Med Chem. 2013;56:8860–71.
McNamara CW, Lee MCS, Lim CS, Lim SH, Roland J, Nagle A, et al. Targeting plasmodium PI(4)K to eliminate malaria. Nature. 2013;504:248–53.
Zhang YK, Plattner JJ, Freund YR, Easom EE, Zhou Y, Gut J, et al. Synthesis and structure-activity relationships of novel benzoxaboroles as a new class of antimalarial agents. Bioorg Med Chem Lett. 2011;21:644–51.
Zhang YK, Plattner JJ, Easom EE, Jacobs RT, Guo D, Freund YR, et al. Benzoxaborole antimalarial agents. Part 5. Lead optimization of novel amide pyrazinyloxy benzoxaboroles and identification of a preclinical candidate. J Med Chem. 2017;60:5889–908.
Zhang YK, Plattner JJ, Easom EE, Jacobs RT, Guo D, Sanders V, et al. Benzoxaborole antimalarial agents. Part 4. Discovery of potent 6-(2-(alkoxycarbonyl)pyrazinyl-5-oxy)-1,3-dihydro-1-hydroxy-2,1-benzoxaboroles. J Med Chem. 2015;58:5344–54.
Sonoiki E, Ng CL, Lee MCS, Guo D, Zhang YK, Zhou Y, et al. A potent antimalarial benzoxaborole targets a Plasmodium falciparum cleavage and polyadenylation specificity factor homologue. Nat Commun. 2017;8:14574.
Pegoraro S, Duffey M, Otto TD, Wang Y, Rösemann R, Baumgartner R, et al. SC83288 is a clinical development candidate for the treatment of severe malaria. Nat Commun. 2017;8:14193.
Leban J, Pegoraro S, Dormeyer M, Lanzer M, Aschenbrenner A, Kramer B. Sulfonyl-phenyl-ureido benzamidines. Bioorg Med Chem Lett. 2004;14:1979–82.
Duffey M, Sanchez CP, Lanzer M. Profiling of the anti-malarial drug candidate SC83288 against artemisinins in Plasmodium falciparum. Malar J. 2018;17:121.
Burgess SJ, Kelly JX, Shomloo S, Wittlin S, Brun R, Liebmann K, et al. Synthesis, structure-activity relationship, and mode-of-action studies of antimalarial reversed chloroquine compounds. J Med Chem. 2010;53:6477–89.
Burgess SJ, Selzer A, Kelly JX, Smilkstein MJ, Riscoe MK, Peyton DH. A chloroquine-like molecule designed to reverse resistance in Plasmodium falciparum. J Med Chem. 2006;49:5623–5.
Wirjanata G, Sebayang BF, Chalfein F, Prayoga, Handayuni I, Noviyanti R, et al. Contrasting ex vivo efficacies of “reversed chloroquine” compounds in chloroquine-resistant Plasmodium falciparum and P. vivax isolates. Antimicrob Agents Chemother. 2015;59:5721–6.
Yuthavong Y, Tarnchompoo B, Vilaivan T, Chitnumsub P, Kamchonwongpaisan S, Charman SA, et al. Malarial dihydrofolate reductase as a paradigm for drug development against a resistance-compromised target. Proc Natl Acad Sci USA. 2012;109:16823–8.
Guiguemde WA, Shelat AA, Bouck D, Duffy S, Crowther GJ, Davis PH, et al. Chemical genetics of Plasmodium falciparum. Nature. 2010;465:311–5.
Floyd DM, Stein P, Wang Z, Liu J, Castro S, Clark JA, et al. Hit-to-lead studies for the antimalarial tetrahydroisoquinolone carboxanilides. J Med Chem. 2016;59:7950–62.
Jiménez-Díaz MB, Ebert D, Salinas Y, Pradhan A, Lehane AM, Myrand-Lapierre ME, et al. (+)-SJ733, a clinical candidate for malaria that acts through ATP4 to induce rapid host-mediated clearance of Plasmodium. Proc Natl Acad Sci USA. 2014;111:E5455–62.
Spillman NJ, Kirk K. The malaria parasite cation ATPase PfATP4 and its role in the mechanism of action of a new arsenal of antimalarial drugs. Int J Parasitol Drugs Drug Resist. 2015;5:149–62.
Boss C, Aissaoui H, Amaral N, Bauer A, Bazire S, Binkert C, et al. Discovery and characterization of ACT-451840: an antimalarial drug with a novel mechanism of action. ChemMedChem. 2016;11:1995–2014.
Bihan AL, de Kanter R, Angulo-Barturen I, Binkert C, Boss C, Brun R, et al. Characterization of novel antimalarial compound ACT-451840: preclinical assessment of activity and dose-efficacy modeling. PLoS Med. 2016;13:e1002138.
Krause A, Dingemanse J, Mathis A, Marquart L, Möhrle JJ, McCarthy JS. Pharmacokinetic/pharmacodynamic modelling of the antimalarial effect of Actelion-451840 in an induced blood stage malaria study in healthy subjects. Br J Clin Pharmacol. 2016;82:412–21.
Charman SA, Arbe-Barnes S, Bathurst IC, Brun R, Campbell M, Charman WN, et al. Synthetic ozonide drug candidate OZ439 offers new hope for a single-dose cure of uncomplicated malaria. Proc Natl Acad Sci USA. 2011;108:4400–5.
Vennerstrom JL, Arbe-Barnes S, Brun R, Charman SA, Chiu FCK, Chollet J, et al. Identification of an antimalarial synthetic trioxolane drug development candidate. Nature. 2004;430:900–4.
Dong Y, Wittlin S, Sriraghavan K, Chollet J, Charman SA, Charman WN, et al. The structure-activity relationship of the antimalarial ozonide Arterolane (OZ277). J Med Chem. 2010;53:481–91.
Dong Y, Chollet J, Matile H, Charman SA, Chiu FCK, Charman WN, et al. Spiro and dispiro-1,2,4-trioxolanes as antimalarial peroxides: charting a workable structure-activity relationship using simple prototypes. J Med Chem. 2005;48:4953–61.
Dong Y, Tang Y, Chollet J, Matile H, Wittlin S, Charman SA, et al. Effect of functional group polarity on the antimalarial activity of spiro and dispiro-1,2,4-trioxolanes. Bioorg Med Chem. 2006;14:6368–82.
Kaiser M, Wittlin S, Nehrbass-Stuedli A, Dong Y, Wang X, Hemphill A, et al. Peroxide bond-dependent antiplasmodial specificity of artemisinin and OZ277 (RBx11160). Antimicrob Agents Chemother. 2007;51:2991–3.
Dong Y, Wang X, Kamaraj S, Bulbule VJ, Chiu FCK, Chollet J, et al. Structure-activity relationship of the antimalarial ozonide Artefenomel (OZ439). J Med Chem. 2017;60:2654–68.
Phyo AP, Jittamala P, Nosten FH, Pukrittayakamee S, Imwong M, White NJ, et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. Lancet Infect Dis. 2016;16:61–9.
Gautam A, Ahmed T, Sharma P, Varshney B, Kothari M, Saha N, et al. Pharmacokinetics and pharmacodynamics of Arterolane maleate following multiple oral doses in adult patients with P. falciparum malaria. J Clin Pharmacol. 2011;51:1519–28.
Valecha N, Krudsood S, Tangpukdee N, Mohanty S, Sharma SK, Tyagi PK, et al. Arterolane maleate plus piperaquine phosphate for treatment of uncomplicated lasmodium falciparum malaria: a comparative, multicenter, randomized clinical trial. Clin Infect Dis. 2012;55:663–71.
Jourdan J, Matile H, Reift E, Biehlmaier O, Dong Y, Wang X, et al. Monoclonal antibodies that recognize the alkylation signature of antimalarial ozonides OZ277 (Arterolane) and OZ439 (Artefenomel). ACS Infect Dis. 2015;2:54–61.
Allman EL, Painter HJ, Samra J, Carrasquilla M, Llinás M. Metabolomic profiling of the malaria box reveals antimalarial target pathways. Antimicrob Agents Chemother. 2016;60:6635–49.
Moehrle JJ, Duparc S, Siethoff C, van Giersbergen PLM, Craft JC, Arbe-Barnes S, et al. First-in-man safety and pharmacokinetics of synthetic ozonide OZ439 demonstrates an improved exposure profile relative to other peroxide antimalarials. Br J Clin Pharmacol. 2013;75:535–48.
McCarthy JS, Baker M, O’Rourke P, Marquart L, Griffin P, van Huijsduijnen RH, et al. Efficacy of OZ439 (Artefenomel) against early Plasmodium falciparum blood-stage malaria infection in healthy volunteers. J Antimicrob Chemother. 2016;71:2620–7.
Plouffe D, Brinker A, McNamara C, Henson K, Kato N, Kuhen K, et al. In silico activity profiling reveals the mechanism of action of antimalarials discovered in a high-throughput screen. Proc Natl Acad Sci USA. 2008;105:9059–64.
Nagle A, Wu T, Kuhen K, Gagaring K, Borboa R, Francek C, et al. Imidazolopiperazines: lead optimization of the second-generation antimalarial agents. J Med Chem. 2012;55:4244–73.
Wu T, Nagle A, Kuhen K, Gagaring K, Borboa R, Francek C, et al. Imidazolopiperazines: hit to lead optimization of new antimalarial agents. J Med Chem. 2011;54:5116–30.
Kuhen KL, Chatterjee AK, Rottmann M, Gagaring K, Borboa R, Buenviaje J, et al. KAF156 Is an antimalarial clinical candidate with potential for use in prophylaxis, treatment, and prevention of disease transmission. Antimicrob Agents Chemother. 2014;58:5060–7.
Rottmann M, McNamara C, Yeung BKS, Lee MCS, Zou B, Russell B, et al. Spiroindolones, a potent compound class for the treatment of malaria. Science. 2010;329:1175–80.
Yeung BKS, Zou B, Rottmann M, Lakshminarayana SB, Ang SH, Leong SY, et al. Spirotetrahydro \(\beta\)-carbolines (spiroindolones): a new class of potent and orally efficacious compounds for the treatment of malaria. J Med Chem. 2010;53:5155–64.
White NJ, Pukrittayakamee S, Phyo AP, Rueangweerayut R, Nosten F, Jittamala P, et al. Spiroindolone KAE609 for falciparum and vivax malaria. N Engl J Med. 2014;371:403–10.
Coteron JM, Marco M, Esquivias J, Deng X, White KL, White J, et al. Structure-guided lead optimization of triazolopyrimidine-ring substituents identifies potent Plasmodium falciparum dihydroorotate dehydrogenase inhibitors with clinical candidate potential. J Med Chem. 2011;54:5540–61.
McCarthy JS, Lotharius J, Rückle T, Chalon S, Phillips MA, Elliott S, et al. Safety, tolerability, pharmacokinetics, and activity of the novel long-acting antimalarial DSM265: a two-part first-in-human phase 1a/1b randomised study. Lancet Infect Dis. 2017;17:626–35.
Nigussie D, Beyene T, Shah NA, Belew S. New targets in malaria parasite chemotherapy: a review. Malaria Contr Elimination. 2015;S1:S1–007.
Jorgensen R, Merrill AR, Andersen GR. The life and death of translation elongation factor 2. Biochem Soc Trans. 2006;34:1–6.
Spillman NJ, Allen RJW, McNamara CW, Yeung BKS, Winzeler EA, Diagana TT, et al. Na\(^+\) Regulation in the malaria parasite Plasmodium falciparum involves the cation ATPase PfATP4 and is a target of the spiroindolone antimalarials. Cell Host Microbe. 2013;13:227–37.
Open Source Malaria Series 4 GitHub Repository. https://github.com/OpenSourceMalaria/Series4. Accessed 17 June 2018.
Voorhis WCV, Adams JH, Adelfio R, Ahyong V, Akabas MH, Alano P, et al. Open source drug discovery with the malaria box compound collection for neglected diseases and beyond. PLoS Pathog. 2016;12:e1005763.
Dennis ASM, Rosling JEO, Lehane AM, Kirk K. Diverse antimalarials from whole-cell phenotypic screens disrupt malaria parasite ion and volume homeostasis. Sci Rep. 2018;8:8795.
Saliba KJ, Kirk K. pH Regulation in the intracellular malaria parasite Plasmodium falciparum. J Biol Chem. 1999;274:33213–9.
Baldwin J, Farajallah AM, Malmquist NA, Rathod PK, Phillips MA. Malarial dihydroorotate dehydrogenase. J Biol Chem. 2002;277:41827–34.
Phillips MA, Lotharius J, Marsh K, White J, Dayan A, White KL, et al. A long-duration dihydroorotate dehydrogenase inhibitor (DSM265) for prevention and treatment of malaria. Sci Transl Med. 2015;7:296ra111.
Yuthavong Y, Yubaniyama J, Chitnumsub P, Vanichtanankul J, Chusacultanachai S, Tarnchompoo B, et al. Malarial (Plasmodium falciparum) dihydrofolate reductase-thymidylate synthase: structural basis for antifolate resistance and development of effective inhibitors. Parasitology. 2005;130:249–59.
Luth MR, Gupta P, Ottilie S, Winzeler EA. Using in vitro evolution and whole genome analysis to discover next generation targets for antimalarial drug discovery. ACS Infect Dis. 2018;4:301–14.
IUPHAR/MMV Guide to Malaria Pharmacology Project. http://www.guidetomalariapharmacology.org/. Accessed 14 Jan 2019.
Authors' contributions
All authors contributed to the writing, editing and proofing of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors thank various contributors for provision of unpublished data: these contributions have been acknowledged in the manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
The authors thank the Australian Research Council and the Medicines for Malaria Venture for funding (LP150101226).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Additional files
Additional file 1.
Compounds reference list. List of SciFinder reference dois for each compound described in the Future section of this review.
Additional file 2.
Biological data for compounds. Tabulation of biological potencies and pharmacokinetic properties for each compound described in Future section of this review.
Additional file 3.
SMILES strings and CID numbers for compounds. List of SMILES strings and CID numbers for every compound described in this review.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tse, E.G., Korsik, M. & Todd, M.H. The past, present and future of anti-malarial medicines. Malar J 18, 93 (2019). https://doi.org/10.1186/s12936-019-2724-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-019-2724-z