- Research
- Open access
- Published:
Malaria among under-five children in Ethiopia: a systematic review and meta-analysis
Malaria Journal volume 21, Article number: 338 (2022)
Abstract
Background
Globally, malaria is among the leading cause of under-five mortality and morbidity. Despite various malaria elimination strategies being implemented in the last decades, malaria remains a major public health concern, particularly in tropical and sub-tropical regions. Furthermore, there have been limited and inconclusive studies in Ethiopia to generate information for action towards malaria in under-five children. Additionally, there is a considerable disparity between the results of the existing studies. Therefore, the pooled estimate from this study will provide a more conclusive result to take evidence-based interventional measures against under-five malaria.
Methods
The protocol of this review is registered at PROSPERO with registration number CRD42020157886. All appropriate databases and grey literature were searched to find relevant articles. Studies reporting the prevalence or risk factors of malaria among under-five children were included. The quality of each study was assessed using the Newcastle–Ottawa Quality Assessment Scale (NOS). Data was extracted using Microsoft Excel 2016 and analysis was done using STATA 16.0 statistical software. The pooled prevalence and its associated factors of malaria were determined using a random effect model. Heterogeneity between studies was assessed using the Cochrane Q-test statistics and I2 test. Furthermore, publication bias was checked by the visual inspection of the funnel plot and using Egger’s and Begg’s statistical tests.
Results
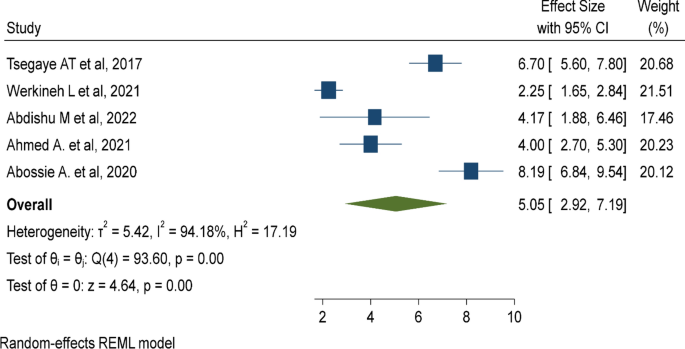
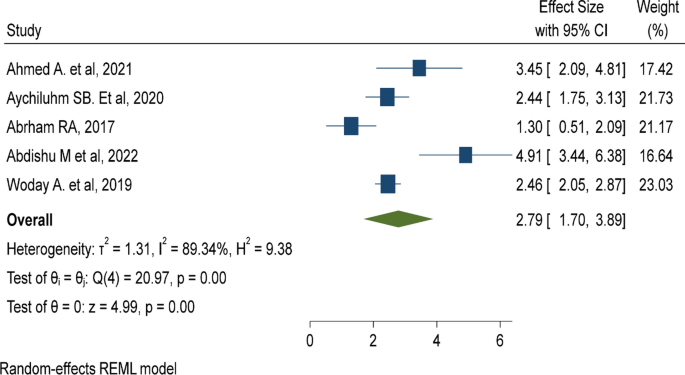
Twelve studies with 34,842 under-five children were included. The pooled prevalence of under-five malaria was 22.03% (95% CI 12.25%, 31.80%). Lack of insecticide-treated mosquito net utilization (AOR: 5.67, 95% CI 3.6, 7.74), poor knowledge of child caretakers towards malaria transmission (AOR: 2.79, 95% CI 1.70, 3.89), and living near mosquito breeding sites (AOR: 5.05, 95% CI 2.92, 7.19) were risk factors of under-five malaria.
Conclusion
More than one in five children aged under five years were infected with malaria. This suggests the rate of under-five malaria is far off the 2030 national malaria elimination programme of Ethiopia. The Government should strengthen malaria control strategies such as disseminating insecticide-treated mosquito nets (ITNs), advocating the utilization of ITNs, and raising community awareness regarding malaria transmission.
Background
Malaria is a major public health concern in tropical and sub-tropical regions of the world, affecting hundreds of millions of people. Nearly 3.2 billion people are at risk of malaria worldwide with a substantial risk among pregnant women and children under five years old. In the year 2020, nearly 241 million people were infected by Plasmodium species and half a million died due to malaria. Evidence suggested that more than 95% of malaria infections and deaths are concentrated in African countries. Similarly, more than 90% of malaria-related infections and deaths occur in sub-Saharan regions [1, 2].
Malaria is a major public health problem in Ethiopia where approximately 68% of the land mass has favourable conditions for malaria transmission and 60% of the population is at risk of the disease [3, 4]. Despite various preventive measures undertaken in the last decades, malaria remains among the top ten causes of under-five morbidity and mortality in Ethiopia [5,6,7,8]. Malaria transmission is highly seasonal and varies significantly with respect to geographical altitude, rainfall and population movement. In addition, due to unstable malaria transmission patterns, Ethiopia is prone to focused and large-scale cyclic malaria epidemics [9].
Studies show that children aged under five years are among the most vulnerable to malaria infections. More than 61% of all malaria deaths worldwide and 80% of sub-Saharan malaria deaths occurred among children under 5 years [10, 11]. Similarly, the highest malaria-related morbidity and mortality in Ethiopia is reported among children under 5 years [12,13,14,15]. The 2019 Ethiopian demographic health survey (EDHS) showed that 59 under-fives died in 1,000 live births due to malaria [16].
Despite inconsistency among existing studies, several factors were associated with high prevalence of malaria among children under 5 years. Insecticide-treated mosquito net (ITN) utilization, presence of forest cover, altitude of residence, household density, living near mosquito breeding sites such as stagnant water, seasonal variation, and housing conditions were major predictors of malaria infection among children aged under 5 years. In addition, the low protective immunity of under-fives make them highly susceptible to malaria infection [17,18,19].
Several malaria elimination strategies have been implemented at national and international levels to control the burden of malaria. Consequently, over 6 million malaria deaths were averted between 2000 and 2015 in African countries. Despite this significant decline, malaria remains a major public health concern in tropical and sub-tropical regions of the world [20,21,22]. Furthermore, there are limited and inconclusive studies in Ethiopia to generate information for action against malaria. There is a considerable discrepancy among the results of existing studies. Therefore, the pooled estimate from the current study will provide a more conclusive result to take evidence-based interventional measures against malaria in under-fives in Ethiopia [23].
Methods
Study design
This study was designed based on the updated guideline of the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA 2020) statements to report the findings [24]. The protocol has been registered at PROSPERO with registration number CRD42020157886. Moreover, the authors have used the guideline of PROSPERO for registering the protocol.
Eligibility criteria
The inclusion criteria for this review and meta-analysis were: (1) studies among under-five children in Ethiopia; (2) observational studies (cross-sectional, case-control, cohort studies, longitudinal studies); (3) studies that report the prevalence or factors of under-five malaria; and, (4) English language articles published in peer-reviewed journals not limited by year of study. However, studies that did not define the age of a child, studies that were not fully accessed or failed to contact the primary author (s), case reports, expert opinions, and qualitative studies were excluded.
Searching strategy
This review and meta-analysis was prepared and presented in accordance to the updated guideline of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA 2020) [24]. The international databases PubMed/MEDLINE, HINARI, African Journal of Online (AJOL), and Google Scholar were accessed to find relevant articles. A Medical Subject Headings (MeSH), keyword terms and phrases were used both in separation and in combination using the Boolean operators “OR” and “AND” to search for eligible articles. The authors have also used snowballing of the references of identified articles for accessing potentially relevant studies (Additional file 1).
The keywords and phrases “under-five children”, “0–59 months old children”, pediatrics, ‘‘preschool children’’, malaria, “Plasmodium falciparum”, “Plasmodium vivax”, “mixed malaria”, “Plasmodium species”, prevalence, incidence, magnitude, burden, proportion, determinants, “risk factors”, predictors, causes, ‘‘associated factors”, and Ethiopia were used in separation or in combination to retrieve relevant articles on malaria in under-fives in Ethiopia.
Study selection
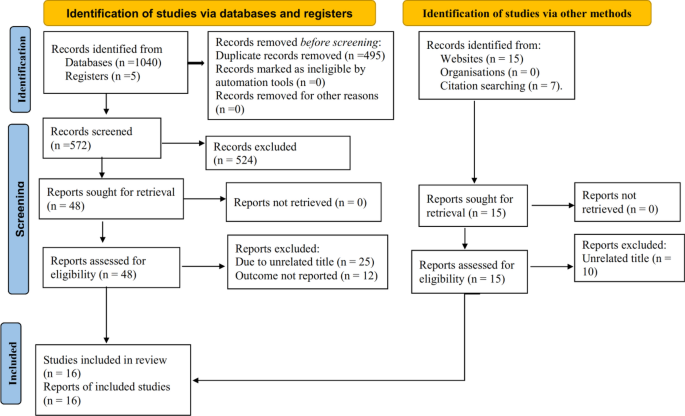
Exhaustively, 1067 studies were retrieved using online databases, reference lists of retrieved articles, and manual searches. All the retrieved articles were exported to Endnote X8 reference managers and 495 articles were removed due to duplication. The title and abstract of the remaining 572 articles were reviewed and 524 articles were removed by title and abstract. Some 48 full articles were assessed for eligibility, which resulted in further exclusion of 36 articles due to lack of outcome reports. Finally, 16 studies were included. Of these 16, 12 studies were used to determine the pooled prevalence of malaria, 11 studies to determine the association between mosquito net utilization and under-five malaria, 5 studies to determine the association between living near mosquito breeding sites and under-five malaria, and 5 studies to determine the association between knowledge of malaria transmission and the incidence of under-five malaria (Fig. 1).
Outcome measurement
The primary outcome of this systematic review and meta-analysis is the pooled prevalence of malaria among under-five children. The pooled prevalence of malaria was calculated by dividing the number of under-fives with malaria by the total number of children included in the study multiplied by 100. The second outcome was determinants of malaria among under-five children, which was estimated by the pooled odds ratio with a 95% confidence interval using a random effect meta-analysis.
Data extraction and management
Data were extracted using Microsoft Excel spreadsheet imported into STATA version 16.0 statistical software for further analysis. Three authors (AW, KD, GB) extracted the data independently. Discrepancies between authors during data extraction were managed through consensus and a fourth author was consulted to resolve disagreements. For each included article, the first author’s last name, year of publication, study setting, study design, study period, sample size, response rate, study population, outcome definition, comparison groups, and effect estimate was recorded.
Quality assessment
The quality of each study was assessed using NOS adapted for meta-analysis. Studies were assessed for representativeness of sample size, non-respondents, ascertainment of exposure, comparability, assessment of the outcome, and statistical tests. Stars were assigned to evaluate study quality, with 9–10 stars indicating “very good” quality, 7–8 stars “good” quality, 5–6 stars “satisfactory” quality, and 0–4 stars “unsatisfactory” quality. Four authors (GB, AW, KD, NA) performed the quality appraisal independently and the average assessment scale was used for the final decision [25].
Publication bias and heterogeneity
Heterogeneity was evaluated using Cochran’s Q statistic with a 5% level of significance and the I2 statistical test. The I2 test statistics of 25, 50 and 75% were declared as low, moderate, and high heterogeneity respectively [26]. The possible risk of publication bias was examined by the inspection of the funnel plot and statistically using Begg’s correlation and Egger’s regression test. Sub-group analysis was conducted by region, sample size and study design to minimize random variation among studies. Besides, sensitivity analysis was performed to examine the influence of a single study on the overall estimate.
Data analysis
The prevalence of malaria was calculated by dividing the number of under-five children with malaria by the total number of children included in the study multiplied by 100. The standard error of the prevalence was calculated using the formula: \(se\;\left(p\right)=\frac{\sqrt{\text{p}(1-\text{p})}}{n}\). Adjusted odds ratio (AOR) with its upper and lower bounds were extracted for significant variables. The standard error of the OR was calculated using the formula: \(\text{SE}\; \log \;(\text{OR})=\left[\frac{UB\;cl-LB\;cl}{2Za/2}\right]\). Then the extracted data were exported into STATA 16.0 statistical software for further analysis. Taking the variability between individual studies and the observed heterogeneity among the included studies, a random effect model analysis was employed. Additionally, sub-group analysis, publications bias and sensitivity analysis were performed.
Results
Study characteristics
Of the 16 included studies, five were in Amhara region, three in Oromia region, four in South Nation Nationality and Peoples of Ethiopia (SNNP) region, two in Binishangulgumz, one in Afar region, and one was a national study. The highest malaria prevalence was reported in Afar region (64.04%) [27], whereas the lowest prevalence was reported in Binishangulgumz (3.93%) [28]. Regarding the study design, 12 studies were cross-sectional, three retrospectives, and one Bayesian study (Table 1).
Prevalence of malaria in under-five children
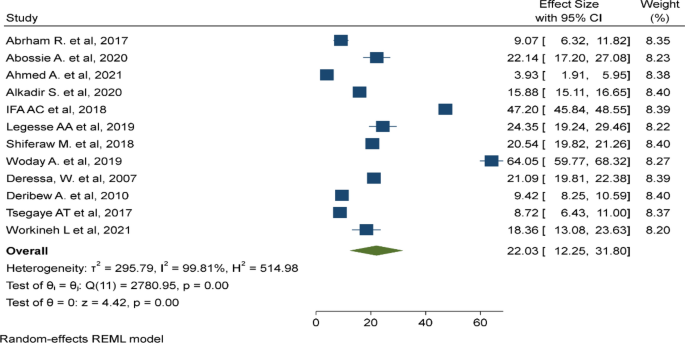
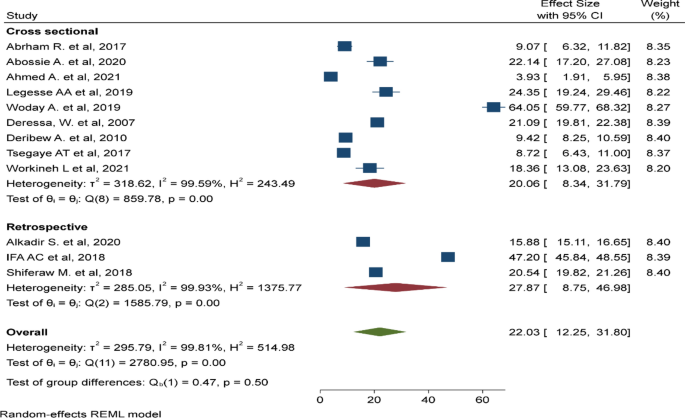
In this meta-analysis, 12 primary studies with 34,842 study participants were included to estimate the pooled prevalence of malaria among under-five children using a random effect model [27,28,29,30,31,32,33,34,35,36,37,38]. The pooled prevalence of malaria among under-five children was 22.03% (95% CI 12.25%, 31.8%, I2: 99.81, P < 0.001) (Fig. 2).
Sub-group analysis
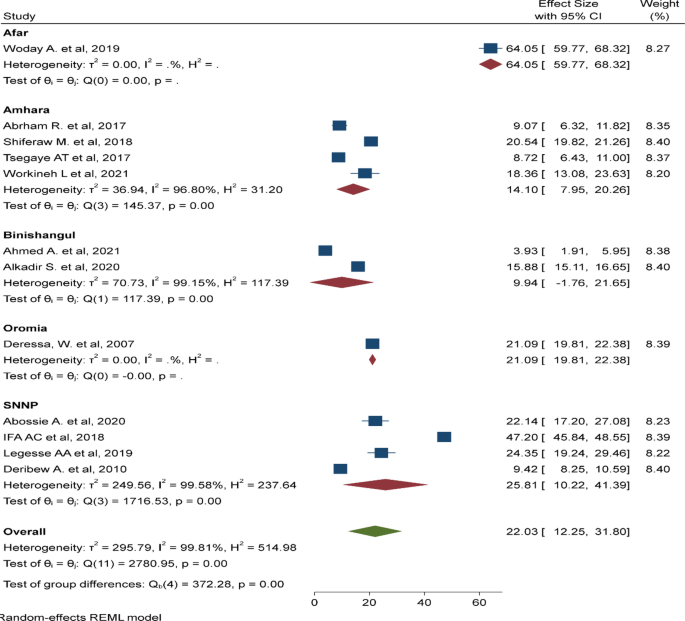
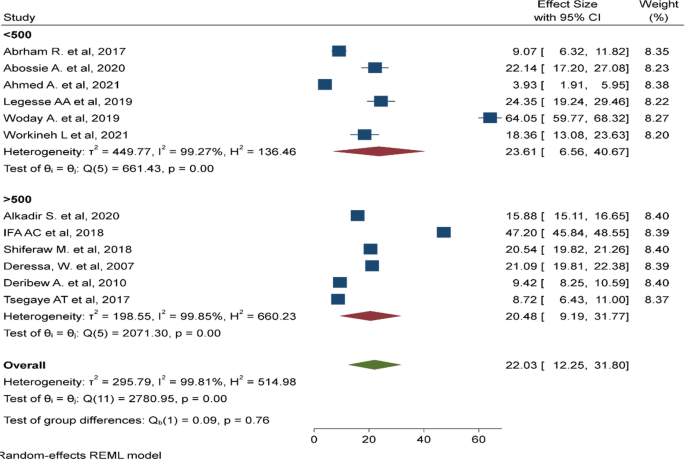
There was a significant heterogeneity among the included studies (I2: 99.81, p < 0.001). As a result, sub-group analyses was done by region (Fig. 3), sample size (Fig. 4), and study design (Fig. 5). The highest pooled prevalence of under-five malaria was reported in SNNP (25.81%, 95% CI 10.22–41.39%) next to a single study in Afar region (64.5%, 95% CI 59.77–68.32%). The pooled prevalence of malaria was higher among studies with a sample size < 500 (23.61%, 95% CI 6.56–40.67%). Similarly, the pooled prevalence of malaria was higher in studies with a retrospective design (27.87%, 95% CI 8.75–46.98%).
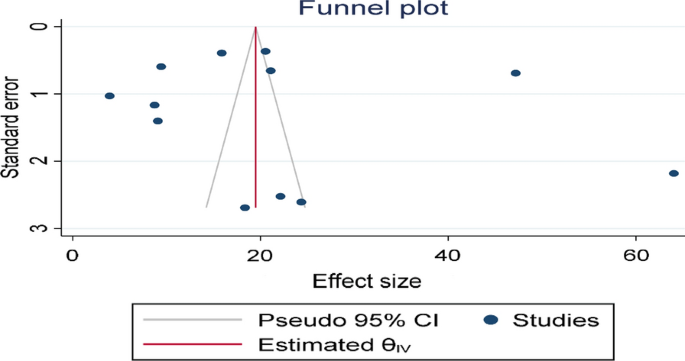
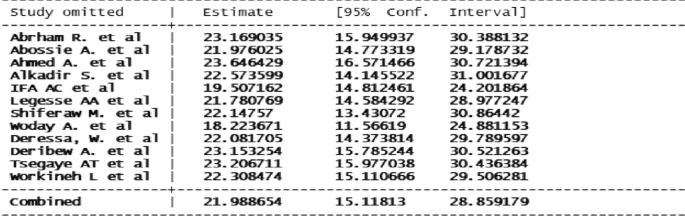
Publication bias and sensitivity analysis
The funnel plot showed a significant publication bias with substantial asymmetry (Fig. 6). The funnel plot is a subjective technique; as a result, objective statistical tests Egger’s test and Begg’s test [39] were done to confirm the presence of publication bias. Consequently, the Egger’s (p = 0.43) and Begg’s statistical tests (p = 0.63) showed no statistical evidence of publication bias. Sensitivity analysis was performed with the random effect model to see the effect of a single study on the overall estimate. However, the analysis showed no evidence for the influence of a single study on the overall estimate (Fig. 7).
Risk factors of malaria in under-five children
Several primary studies were included to determine the pooled factors associated with malaria among children age under 5 years. Eleven primary studies were included to assess the association between ITN utilization, five studies for assessing the association between living near mosquito breeding sites, and five studies to determine the relationship between knowledge of malaria transmission and the prevalence of malaria among under-five children.
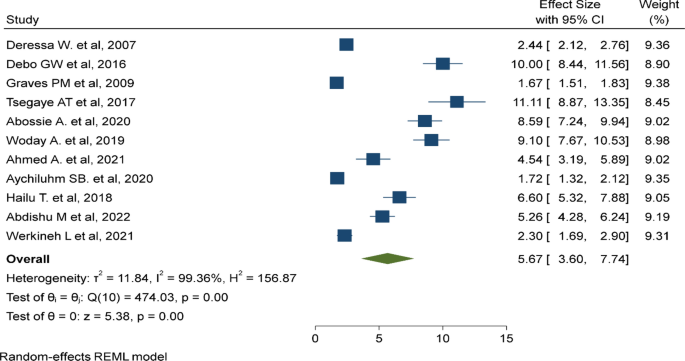
Insecticide-treated mosquito net utilization
In this study, 11 primary studies were included to assess the association of ITN utilization and the prevalence of malaria among children aged under 5 years [27, 28, 30, 35, 37, 38, 40,41,42,43,44]. Children age under 5 years who did not utilize an ITN were nearly 6 times (AOR: 5.67, 95% CI 3.6–7.74) more likely to have malaria than children who did utilize an ITN (Fig. 8).
Living near mosquito breeding sites
In this meta-analysis, five primary studies were included to assess the association between living near mosquito breeding sites and the rate of malaria in under-five children [28, 30, 37, 38, 44]. which was five times (AOR: 5.05, 95% CI 2.92–7.19) more likely to be infected by malaria parasites compared to children living near a non-breeding site (Fig. 9).
Knowledge of malaria transmission
Five primary studies were included to determine the effect of knowledge of child caretakers about malaria transmission on the incidence of under-five malaria [27,28,29, 42, 44], which showed that under-five children with poor knowledge of caretakers toward malaria transmission were nearly three times (AOR: 2.79, 95% CI 1.7–3.89) at high risk of malaria compared to their counterparts (Fig. 10).
Discussion
This study explores and synthesizes the available evidence on malaria in children under 5 years old and its associated factors in Ethiopia. By gathering, synthesizing, and pooling available studies, the finding provides strong evidence on under-five malaria in Ethiopia. The finding revealed that more than one in five children are infected with malaria Plasmodium species. The finding warned the 2030 national malaria elimination programme in Ethiopia [45] needs to emphasize malaria control strategies in the country.
In this study, 22.03% (95% CI 12.25%, 31.80%) under-five children were infected with malaria. The finding is comparable to the pooled estimate in sub-Saharan countries (18.8%) [46], (21%) [47], and (26%) [48], the national malaria survey in Gambella (21%) [49], a study in Uganda (19.04%) [50], the national malaria survey in Ghana (21%) [51], and the national malaria survey in Nigeria (27%) [52]. These findings pointed out that malaria is still a concern for children under 5 years old. The reason could be their low protective immunity makes them highly susceptible to malaria infection, and could be associated with poor malaria control strategies or lack of monitoring and evaluation of malaria control programmes.
The finding shows a nearly 16-fold higher estimate than the national malaria indicator survey in Ethiopia (1.4%) [49]. The Government of Ethiopia need to strengthen malaria control strategies. The finding is threefold higher than the demographic and health survey in Tanzania (7%) [53] and the malaria indicator survey in Kenya (6%) [54]. The reason could be demographic health surveys and malaria indicator surveys are conducted at national level, including low malaria-endemic areas, which thereby lower the report of under-five malaria. However, studies included in this meta-analysis were conducted in high malaria areas of Ethiopia which might increase the prevalence of under-five malaria.
Conversely, the finding was lower than the report in sub-Saharan countries (36%) [55], a study in Malawi (37%) [56], the malaria indicator survey in Liberia (45%) [57], the malaria indicator survey in south Sudan (32%) [58], and a meta-analysis in the Democratic Republic of the Congo (37.4%) [59]. The possible explanation for the discrepancy could be countries might have different malaria monitoring programmes and different levels of achievements in malaria control strategies. The reason could also be due to the fact that Ethiopia had low malaria prevalence compared to most other malaria-endemic countries in Africa [45].
Lack of access to or non-utilization of ITNs is a risk factor for higher prevalence of malaria among under-five children, which is similar to the study in Ethiopia [42], a study in Malawi [60], a study in sub-Saharan countries [47], and a study in Uganda [61]. The reason is the fact that children who utilize ITNs are not exposed to Plasmodium species and are less likely to get infected by the parasite. The Government should disseminate ITNs and advocate utilization to prevent high malaria transmission among under-five children.
Poor knowledge of child caretakers about malaria transmission increases the likelihood of malaria infection. The finding is similar to studies in sub-Saharan countries [62], in Rwanda [63], Ghana [64], Uganda [50], Malawi [56], and Nigeria [65]. The reason could be child caretakers who are not aware of malaria transmission are less likely to protect their child from Plasmodium species. Community awareness regarding malaria transmission and its prevention should be strengthened.
Residing near mosquito breeding sites such as stagnant water increases malaria transmission. The finding is similar to the pooled estimate in sub-Saharan countries [46], studies in Ethiopia [66], Malawi [67], South Africa [68], and Nigeria [65]. The reason is mosquitoes can multiply and survive in stagnant and unprotected water sources. As a result, under-five children living near these areas are at higher risk of malaria infection. Cleaning and removing mosquito breeding sites is advisable to reduce malaria in under-fives in Ethiopia.
Strength and limitations of the study
A limitation of the study is pooling prevalence and odds ratio despite high heterogeneity. There are outliers in the included studies such as the study from Afar region this might result in an exaggerated pooled estimate. Another limitation of the study is its narrow scope, which included studies involving only children aged under 5 years. In addition, only a few factors were considered by excluding factors that were reported in a few studies this might cause bias on the factors of under-five malaria. Similarly, excluding articles that were published other than in English language might cause publication bias.
Conclusion
The finding revealed that more than one in five children aged under 5 years were infected with malaria. The risk factors identified are mostly preventable, including ITN under-utilization, living near mosquito breeding sites, and poor knowledge of malaria transmission and its prevention methods by caretakers. The Government should strengthen malaria control strategies such as eradicating mosquito breeding sites, ensure access to ITNs for all under-five children living in malaria-endemic areas, and raise awareness regarding malaria transmission and its preventative methods.
Availability of data and materials
All materials and data related to this article are included in the main document of the manuscript.
Abbreviations
- EDHS:
-
Ethiopian Demographic and Health Survey
- ITN:
-
Insecticide-treated nets
- LMICs:
-
Low and Middle-Income Countries
- MeSH:
-
Medical Subject Headings
- NOS:
-
Newcastle–Ottawa Quality Assessment Scale
- PECO:
-
Population, Exposure, Comparison, and Outcome
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- SNNP:
-
South Nation Nationality and Peoples
- WHO:
-
World Health Organization
References
WHO. World malaria report. Geneva: World Health Organization; 2017.
WHO. World-malaria-report-2016. Geneva: World Health Organization; 2016.
Taffese HS, Hemming-Schroeder E, Koepfli C, Tesfaye G, Lee M-C, Kazura J, et al. Malaria epidemiology and interventions in Ethiopia from 2001 to 2016. Infect Dis Poverty. 2018;7:103.
Ethiopian Public Health Institute. Ethiopian malaria indicator survey 2015 (EMIS-2015). Ethiopia, Addis Ababa; 2016.
United Nations. The millenium development goals 2015 report. New York; 2015.
Hajia Y, Fogartyb. AW, Deressa W. Prevalence and associated factors of malaria among febrile children in Ethiopia: a cross-sectional health facility-based study. Acta Trop. 2016;155:63–70.
Tadesse F, Fogarty AW, Deressa W. Prevalence and associated risk factors of malaria among adults in East Shewa Zone of Oromia Regional State, Ethiopia: a cross-sectional study. BMC Public Health. 2018;18:25.
Federal Ministry of Finance and Economic Development. Assessing progress towards the millenium development goals: Ethiopia MDGs report 2012. Addis Ababa, Ethiopia; 2012.
Federal Ministry of Health. Health and health related indicators. Addis Ababa, Ethiopia; 2013.
Kassam R, Sekiwunga R, MacLeod D, Tembe J, Liow E. Patterns of treatment-seeking behaviors among caregivers of febrile young children: a Ugandan multiple case study. BMC Public Health. 2016;16:160.
WHO. World malaria report 2019. Geneva: World Health Organization; 2019.
Ashton RA, Kefyalew T, Tesfaye G, Pullan RL, Yadeta D, Reithinger R, et al. School-based surveys of malaria in Oromia Regional State, Ethiopia: a rapid survey method for malaria in low transmission settings. Malar J. 2011;10:25.
Ayalew S. The prevalence of malaria and the associated risk factors in Jiga area, Northwest Ethiopia. Thesis, Addis Ababa University; 2014.
Debo GW, Kassa DH. Prevalence of malaria and associated factors in Benna Tsemay district of pastoralist community, southern Ethiopia. Trop Dis Travel Med Vaccines. 2016;2:16.
Molla E, Ayele B. Prevalence of malaria and associated factors in Dilla Town and the surrounding rural areas, Gedeo Zone, southern Ethiopia. J Bacteriol Parasitol. 2015;6:5.
Ethiopian Public Health Institute (EPHI) and ICF. Ethiopia mini demographic and health survey 2019: key indicators. Rockville, Maryland, USA, Addis Ababa, Ethiopia; 2019.
Roberts D, Matthews G. Risk factors of malaria in children under the age of five years old in Uganda. Malar J. 2016;15:246.
Tassew A, Hopkins R, Deressa W. Factors influencing the ownership and utilization of long-lasting insecticidal nets for malaria prevention in Ethiopia. Malar J. 2017;16:262.
Central Statistical Agency. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia; 2017.
Federal Ministry of Health. Health sector development program IV (2010/11–2014/15) final draft. Addis Ababa, Ethiopia; 2010.
Federal Ministry of Health. Health sector transformation plan (HSTP 2016–2020). Addis Ababa, Ethiopia; 2015.
United Nations. Transforming our world: the 2030 agenda for sustainable development. New York; 2015. https://stg-wedocs.unep.org/bitstream/handle/20.500.11822/11125/unepswiosm1inf7sdg.pdf?sequence=1.
Jima D, Wondabeku M, Alemu A, Teferra A, Awel N, Deressa W, et al. Analysis of malaria surveillance data in Ethiopia: what can be learned from the Integrated disease surveillance and response system? Malar J. 2012;11:330.
MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.https://doi.org/10.1136/bmj.n71.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Woday A, Mohammed A, Gebre A, Urmale K. Prevalence and associated factors of malaria among febrile children in Afar region, Ethiopia: a health facility based study. Ethiop J Health Sci. 2019;29:5.
Ahmed A, Mulatu K, Elfu B. Prevalence of malaria and associated factors among under-five children in Sherkole refugee camp, Benishangul-Gumuz region, Ethiopia. A cross-sectional study. PLoS ONE. 2021;16:e0246895.
Abrham R. Preventing malaria among under five children in Damot Gale Woreda, Wolayta Zone, Ethiopia: the role of parents knowledge and treatment seeking. Prim Health Care. 2017;7:284.
Abossie A, Yohanes T, Nedu A, Tafesse W, Damitie M. Prevalence of malaria and associated risk factors among febrile children under five years: a cross-sectional study in Arba Minch Zuria district, south Ethiopia. Infect Drug Resist. 2020;13:363.
Alkadir S, Gelana T, Gebresilassie A. A five year trend analysis of malaria prevalence in Guba district, Benishangul-Gumuz regional state, western Ethiopia: a retrospective study. Trop Dis Travel Med Vaccines. 2020;6:18.
Chemeda Ifa A. Trend in malaria prevalence among children under five years of age in the Hadiya Zone, southern Ethiopia: a five-year retrospective study. Fam Med Prim Care Rev. 2018;20:337–40.
Legesse AA. Prevalence of malaria and associated risk factors among febrile children under 5 years in Gamo-Gofa, Ethiopia: an institutional based cross sectional study. 30th EPHA annual conference; 2019.
Shiferaw M, Alemu M, Tedla K, Tadesse D, Bayissa S, Bugssa G. The prevalence of malaria in Tselemti Wereda, North Ethiopia: a retrospective study. Ethiop J Health Sci. 2018;28:5.
Deressa W, Ali A, Berhane Y. Household and socioeconomic factors associated with childhood febrile illnesses and treatment seeking behaviour in an area of epidemic malaria in rural Ethiopia. Trans R Soc Trop Med Hyg. 2007;101:939–47.
Deribew A, Alemseged F, Tessema F, Sena L, Birhanu Z, Zeynudin A, et al. Malaria and under-nutrition: a community based study among under-five children at risk of malaria, south-west Ethiopia. PLoS ONE. 2010;5:e10775.
Tsegaye AT, Ayele A, Birhanu S. Prevalence and associated factors of malaria in children under the age of five years in Wogera district, northwest Ethiopia: a cross-sectional study. PLoS ONE. 2021;16:e0257944.
Workineh L, Lakew M, Dires S, Kiros T, Damtie S, Hailemichael W, et al. Prevalence of malaria and associated factors among children attending health institutions at South Gondar Zone, Northwest Ethiopia: a cross-sectional study. Glob Pediatr Health. 2021;8:2333794X211059107.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Debo GW, Kassa DH. Prevalence of malaria and associated factors in Benna Tsemay district of pastoralist community, Southern Ethiopia. Trop Dis Travel Med Vaccines. 2016;2:9.
Graves PM, Richards FO, Ngondi J, Emerson PM, Shargie EB, Endeshaw T, et al. Individual, household and environmental risk factors for malaria infection in Amhara, Oromia and SNNP regions of Ethiopia. Trans R Soc Trop Med Hyg. 2009;103:1211–20.
Aychiluhm SB, Gelaye KA, Angaw DA, Dagne GA, Tadesse AW, Abera A, et al. Determinants of malaria among under-five children in Ethiopia: Bayesian multilevel analysis. BMC Public Health. 2020;20:1468.
Hailu T, Alemu M, Mulu W, Abera B. Incidence of Plasmodium infections and determinant factors among febrile children in a district of Northwest Ethiopia; a cross-sectional study. Trop Dis Travel Med Vaccines. 2018;4:6.
Abdishu M, Gobena T, Damena M, Abdi H, Birhanu A. Determinants of malaria morbidity among school-aged children living in East Hararghe Zone, Oromia, Ethiopia: a community-based case–control study. Pediatr Health Med Ther. 2022;13:183.
Federal Democratic Republic of Ethiopia Ministry of Health. National malaria strategic plan 2021–2025. Addis Ababa, Ethiopia; 2020.
Yang D, He Y, Wu B, Deng Y, Li M, Yang Q, et al. Drinking water and sanitation conditions are associated with the risk of malaria among children under five years old in sub-Saharan Africa: a logistic regression model analysis of national survey data. J Adv Res. 2019;21:1–13.
Tusting LS, Gething PW, Gibson HS, Greenwood B, Knudsen J, Lindsay SW, et al. Housing and child health in sub-Saharan Africa: a cross-sectional analysis. PLoS Med. 2020;17:e1003055.
Taylor C, Namaste SM, Lowell J, Useem J, Yé Y. Estimating the fraction of severe malaria among malaria-positive children: analysis of household surveys in 19 malaria-endemic countries in Africa. Am J Trop Med Hyg. 2021;104:1375.
Federal Democratic Republic of Ethiopia Ministry of Health. Ethiopia national malaria indicator survey 2015. Addis Ababa, Ethiopia; 2016.
Wanzira H, Katamba H, Okullo AE, Agaba B, Kasule M, Rubahika D. Factors associated with malaria parasitaemia among children under 5 years in Uganda: a secondary data analysis of the 2014 malaria indicator survey dataset. Malar J. 2017;16:191.
Ghana Statistical Service (GSS). Ghana Health Service (GHS), and ICF. Ghana malaria indicator survey 2016. Accra, Ghana, and Rockville, USA. 2017.
National Malaria Elimination Programme (NMEP), National Population Commission (NPopC). National Bureau of Statistics (NBS), and ICF International. Nigeria malaria indicator survey 2015. Abuja, Nigeria; 2016.
Ministry of Health. Community Development, Gender, Elderly and Children [Tanzania Mainland], Ministry of Health [Zanzibar], National Bureau of Statistics, Office of the Chief Government Statistics, and ICF. Tanzania malaria indicator survey (TMIS) 2017: malaria atlas. Dar se Saalam, Tanzania, and Rockville, USA; 2017.
Division of National Malaria Programme [Kenya] and ICF. Kenya malaria indicator survey 2020. Nairobi, Kenya and Rockville, Maryland, USA; 2021.
Berendsen ML, Van Gijzel SW, Smits J, De Mast Q, Aaby P, Benn CS, et al. BCG vaccination is associated with reduced malaria prevalence in children under the age of 5 years in sub-Saharan Africa. BMJ Glob Health. 2019;4:e001862.
Gaston RT, Ramroop S. Prevalence of and factors associated with malaria in children under five years of age in Malawi, using malaria indicator survey data. Heliyon. 2020;6:e03946.
National Malaria Control Programme [Liberia], Ministry of Health, Liberia Institute of Statistics and Geo-Information Services, and ICF. Liberia malaria indicator survey 2016. Liberia, Monrovia and Rockville, USA; 2017.
Ministry of Health, Republic of South Sudan. Malaria Indicator Survey (MIS) 2017. Juba, South Sudan; 2017.
Levitz L, Janko M, Mwandagalirwa K, Thwai KL, Likwela JL, Tshefu AK, et al. Effect of individual and community-level bed net usage on malaria prevalence among under-fives in the Democratic Republic of Congo. Malar J. 2018;17:39.
Chitunhu S, Musenge E. Direct and indirect determinants of childhood malaria morbidity in Malawi: a survey cross-sectional analysis based on malaria indicator survey data for 2012. Malar J. 2015;14:265.
Kooko R, Wafula ST, Orishaba P. Socio-economic determinants of malaria prevalence among under five children in Uganda: evidence from 2018–19 Uganda malaria indicator survey. J Vector Borne Dis. 2022. Online ahead of print.
Obasohan PE, Walters SJ, Jacques R, Khatab K. A scoping review of selected studies on predictor variables associated with the malaria status among children under five years in sub-Saharan Africa. Int J Environ Res Public Health. 2021;18:2119.
Ayele DG, Zewotir TT, Mwambi HG. The risk factor indicators of malaria in Ethiopia. Malar J. 2012;11:195.
Ejigu BA, Wencheko E. Spatial prevalence and determinants of malaria among under-five Children in Ghana. MedRxiv. 2021. https://doi.org/10.1101/2021.03.12.21253436.
Adefemi K, Awolaran O, Wuraola C. Social and environmental determinants of malaria in under five children in Nigeria: a review. Int J Community Med Public Health. 2015;2:345–50.
McMahon A, Mihretie A, Ahmed AA, Lake M, Awoke W, Wimberly MC. Remote sensing of environmental risk factors for malaria in different geographic contexts. Int J Health Geograph. 2021;20:28.
Hajison PL, Feresu SA, Mwakikunga BW. Malaria in children under-five: a comparison of risk factors in lakeshore and highland areas, Zomba district, Malawi. PLoS ONE. 2018;13:e0207207.
Adeola AM, Botai O, Olwoch JM, Rautenbach CdW, Adisa O, Taiwo O, et al. Environmental factors and population at risk of malaria in Nkomazi municipality, South Africa. Trop Med Int Health. 2016;21:675–86.
Acknowledgements
We would like to thank Wollo University’s librarian and information and communication technology (ICT) center staff for availing us of uninterrupted internet connection. We also acknowledge PROSPERO for registration of this protocol.
Funding
No funding was used.
Author information
Authors and Affiliations
Contributions
GB, AWT, KDT, NA, and LT have conceived the title and written the protocol. GB, AWT, and KDT have performed the search strategy. GB, NA, and LT performed the quality assessment, data extraction, and the analysis. All authors have been involved in the final write-up of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA 2020 Checklist for reporting the finding.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Biset, G., Tadess, A.W., Tegegne, K.D. et al. Malaria among under-five children in Ethiopia: a systematic review and meta-analysis. Malar J 21, 338 (2022). https://doi.org/10.1186/s12936-022-04370-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04370-9