- Research
- Open access
- Published:
Effectiveness of seasonal malaria chemoprevention in three regions of Togo: a population-based longitudinal study from 2013 to 2020
Malaria Journal volume 21, Article number: 400 (2022)
Abstract
Background
In 2012, the World Health Organization (WHO) recommended seasonal malaria chemoprevention (SMC) in areas of high seasonal transmission. Though implemented since 2013, the effectiveness of SMC in Togo was never evaluated.
Methods
This study concerned routine data from 2013 to 2020 mass SMC campaigns for children under five in all health facilities of three Regions of Togo. Treatment coverage, reasons for non-treatment, and SMC-attributable adverse reactions were analysed per year and treatment round. Random effect logistic models estimated SMC effectiveness per health district, year, and treatment round.
Results
The overall coverage was 98% (7,971,877 doses for 8,129,668 children). Contraindication was the main reason for non-administration. Over the study period, confirmed malaria cases decreased from 11,269 (1st round of 2016) to 1395 (4th round of 2020). Only 2,398 adverse reactions were reported (prevalence: 3/10,000), but no severe Lyell syndrome or Stevens-Johnson-type skin reaction. Compared to 2016, malaria prevalence decrease was estimated at 22.6% in 2017 (p < 0.001) and 75% in 2020 (p < 0.001). SMC effectiveness ranged from 76.6% (2nd round) to 96.2% (4th round) comparison with the 1st round.
Conclusions
SMC reduced significantly malaria cases among children under five. The results reassure all actors and call for effort intensification to reach the WHO goals for 2030.
Background
In 2019, the World Health Organization (WHO) estimated at nearly 229 million the number of malaria cases in 87 endemic countries [1]. In sub-Saharan Africa, nearly 70% of the deaths due to malaria occur in children under five [2] and, whereas the global incidence of malaria decreased by 27% between 2000 and 2015, it decreased by only 2% between 2015 and 2019, indicating a declining progress since 2015 [1].
The progress in the fight against malaria is probably due to robust strategies for prevention, diagnosis, treatment, and surveillance in endemic areas. Among these strategies, seasonal malaria chemoprevention (SMC), carried out since 2012 seems to have considerably reduced malaria morbidity and mortality, especially in children under five [3].
The effectiveness of SMC has been proven by the results of several clinical trials conducted between 2002 and 2011 in areas of high seasonal transmission of malaria in sub-Saharan Africa [4,5,6,7,8,9,10]. One conclusion of these studies was that “monthly administration of SMC with sulfadoxine-pyrimethamine and amodiaquine (SP + AQ) for up to three or four months during the season of high malaria transmission in children aged 3–59 months: (i) prevents about 75% of all malaria attacks; (ii) prevents about 75% of severe malaria episodes; (iii) reduces the incidence of anaemia; (iv) curbs the increase in clinical malaria during the following season; and (v) would not lead to serious adverse events” [3, 10, 11].
In Togo, malaria is still endemic in all health districts. The entire population is at risk but children under five are the most vulnerable. Currently, Togo is among the countries with stable transmission but with seasonal increases from June to October in the northern half of the country and from April to July and then from August to October in the southern half [12]. In agreement with the recommendations of the WHO, Togo has adopted the SMC as a high impact intervention to help reduce malaria morbidity and mortality in children under five. This intervention has been included in the National Malaria Control Programme (NMCP) and in the 2017–2023 National Strategic Plan.
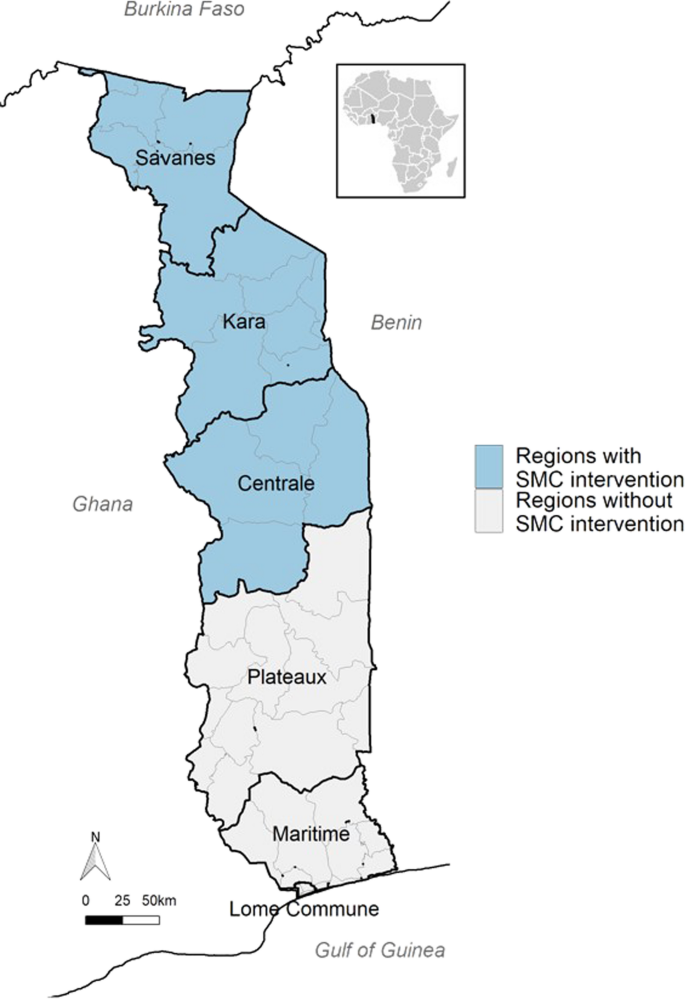
Because of their epidemiological and pluviometry data, the northern regions of Togo (Savanes, Kara, and Centrale; 16 health districts > 60% of that area malaria cases from July to October) were the first to implement SMC. To ensure the follow-up of that strategy, the Ministry of Health and Public Hygiene (through the NMCP) has set up, since 2013, a system to collect SMC data in those regions. However, despite their availability, these data have never been analysed to assess the effectiveness of SMC as in some other countries [13,14,15,16].
This longitudinal study analysed routine data from SMC mass campaigns. It aimed to measure the effectiveness of SMC in children aged 3–59 months living in Savanes, Kara, and Centrale regions of Togo from 2013 to 2020.
Methods
Study type and setting
The study examined data relative to children aged 3–59 months in three regions of Togo (Savanes, Kara, and Centrale) who received SMC according to the WHO recommendation of March 2012 [3]. These data were prospectively collected by the NMCP during the seasons of heavy rainfall over a maximum of four consecutive months (or rounds) per year (July–October) between 2013 and 2020.
The study area of 33,525 km2 (nearly 60% of Togo) is surrounded by Burkina Faso, Benin, Ghana, and Plateaux Region of Togo (Fig. 1). It includes three out of the six Regions of Togo, which corresponds to 16 health districts out of 44 and 324 health centers out of 987 in the whole of Togo. In 2019, the study area was home to nearly 2,829,887 people; i.e., nearly 30% of the Togolese population.
From a climatic point of view, the study area is characterized by two seasons: a dry season from November to May and a rainy season from June to October with heavy rainfall between July and September. It is during the latter period that upsurges in malaria cases are seen and that SMC is administered.
Administration of SMC
Usually, a SMC campaign includes a maximum of four treatment rounds over four consecutive months. During each round, SMC is administered by hired community health workers (CHWs) who use two community approaches: (i) a ‘door-to-door’ approach by pairs of CHWs who visit households to identify children under five and administer the drugs; and (ii) a ‘fixed-post’ approach in health facilities to treat target children absent from home at the time of the CHWs’ visit.
A treatment round consists in administering one dose of sulfadoxine-pyrimethamine (SP) and three doses of amodiaquine (AQ) over three days. SP and the first dose of AQ are given under the supervision of a CHW; the other doses of AQ are given on the next two days by a parent or a guardian.
Before their visits to the households, the CHWs receive specific training. Besides, the NMCP ensures that SMC beneficiaries understand the objectives of the treatment. This is usually done through awareness meetings with local leaders and dissemination of messages through various public media. During an SMC campaign, the supervision is generally provided by the managers of the health facilities, the districts, the Regions, and the NMPC.
Data collection
Sociodemographic data, administrative follow-up data, and information on adverse events were collected by 5787 CHWs from tools such as SMC cards, tally sheets, SMC treatment records, supervision forms, and adverse event count sheets. The CHWs had to report on specific sheets all adverse events occurring after treatment administration. These data were then compiled and validated by 324 health facility managers and sent to the 16 district managers. At the district level, these data were validated and transmitted to the three directors of the target Regions then to the NMCP. To improve the quality of those data and estimate the treatment coverage, the NMCP carried out community surveys at the end of each round.
Operational definitions
Malaria prevalence is the number of children with malaria (children with positive ‘rapid diagnostic test’ (RDT) plus children already treated for malaria) divided by the number of children identified in the eligible age range.
SMC coverage is the ratio of the number of children aged 3–59 months who received all SMC doses per round, district, or region to the number of eligible children identified per round, district, or region, respectively. Previously, expected numbers of children aged 3–59 months and eligible for a SMC campaign within a given region were provided by a statistics department supervised by the Togolese Ministry of Health and actual numbers of eligible children at implementation of each SMC round (thus, year) was obtained by the CHWs.
The effectiveness of a SMC campaign was defined as the percent reduction in malaria cases in each of the two or three last months of a campaign in comparison with the first month. Precisely, over the first year of SMC, a random sample of children who had received a first round underwent parasitemia (RDT) tests at the times of administration of the second, third, and fourth round to determine the proportion of infected children one month after the end of a year’s SMC. This survey included only children whose caregivers confirmed the absence of consumption of other antimalarial drugs over each month following each round. The same survey was repeated in each of the following years. The yearly effectiveness was defined as the percent reduction in malaria cases for each year between 2017 and 2020, in comparison with year 2016. The numbers of malaria cases were obtained via health facilities and CHWs only (no external sources including pharmacies, NGOs), the proof being a positive RDT or a thick-blood-film test.
A SMC-related adverse event is any unexpected reaction in a child who received SMC treatment: vomiting, skin reactions (itching, hives), abdominal pain, somnolence, or jaundice. In Togo, cases of adverse events in children less than five are usually reported by the CHWs when administering the next round. In case an adverse event occurred soon after drug administration, the caregiver was asked either to inform the CHW (who generally lives in the same area) or visit the nearest health facility where the event is then reported on a specific sheet. Later, all adverse events are collected centrally for statistical purposes.
Statistical analysis
The prevalence of observed malaria cases in children was modeled using a logistic mixed regression model. Separate fixed effects for ‘year’ (reference year: 2016) and ‘round’ (reference round: first round of a campaign) were estimated using indicator variables and expressed as Odds Ratios (ORs). ‘Year’ and ‘round’ effects were entered as random effects and assumed to vary randomly according to the Region, the district, and the health facility. Effectiveness was calculated as 1 − (ORyear i, round j) with year 2016 and 1st round as references. This can be interpreted as the percent reduction of malaria prevalence. A second model was built including years 2013 to 2020.
The analyses used package lme4 and function glmer in R software (R Core Team, 2017; R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Ethics and regulations
This study was approved in 2017 by the Ministry of Health and Public Hygiene of Togo (Memorandum No. 280/17/SPS/CAB/SG/DGPIS/DPP/DER). The data collected, compiled, and stored by the NMCP did not require obtaining informed consents.
Results
Participant health facilities
At the launch of SMC in Togo (Savanes Region, 2013), only 55 health facilities participated. Three years later, SMC was extended to Kara and Centrale Regions; the number of participant health facilities increased then from 301 in 2016 to 324 in 2020. Kara was the Region that participated the most (128 health facilities in 2020) and Tchaoudjo district in Centrale was the most represented district (36 health facilities yearly since 2016) (Additional file 2: Table S1).
Target children identification
Between 2013 and 2020, the number of registered children in all three Regions increased by 4.6 times (110,354 to 510,242). Overall, Savanes had the highest number of children. In 2016, Centrale, Kara, and Savanes Centrale identified 110,067; 130,936; and 155,039; children; respectively. In 2020, those regions identified 138,743; 171,348; and 200,151; children; respectively (Additional file 3: Table S2).
Treatment administration
Since the implementation of SMC in Togo, 7,971,877 treatments have been administered to eligible children in the three Regions. Between 2013 and 2020, the number of children treated increased by 5.7 times (from 87,918 to 502,275). In 2016, 106,273 children were treated in Centrale; 125,140 in Kara; and 150,815 in Savanes. In 2020, the same Regions treated 135,861; 168,017; and 198,397; children; respectively (Table 1).
SMC coverage
From 2013 to 2020, the SMC coverage rate exceeded the objective of the WHO (at least 95%); it was higher than 98% in all regions. However, there were some differences between districts; e.g., 99% in Blitta, Kéran, and Oti vs. 96% in Kpendjal. The lowest coverage of 80% was observed in Savanes in 2013 (the year SMC was launched in Togo) because several health facilities experienced shortage of drugs (Table 2).
Reasons for not administering SMC
Children who did not receive SMC represented 1.9% of all children identified in the study area. The main reasons were febrile state and positive RDT or intake of artemether-lumefantrine tablets (Coartem® or Riamet®) (35%), absence from home at the time of the CHW’s visit (28.9%), current malaria treatment (10.7%), and current cotrimoxazole intake (6.7%). The reason could not be found in 15 2% of cases (Additional file 4: Table S3).
Side effects
On 7,971,877 target children treated from 2013 to 2020, the safety reports indicated 2,398 adverse reactions, which is an overall prevalence of 3 per 10,000 children treated. The most frequent adverse events were: vomiting (66.1%), drowsiness (11.2%), rash (10.2%), and abdominal pain (5.2%). No severe skin reaction (such as Stevens-Johnson or Lyell syndrome) was reported (Additional file 5: Table S4).
SMC effectiveness
The study showed significant reductions in malaria cases both at round and year levels.
The number of confirmed malaria cases among identified target children dropped from 11,267 cases (2.8% prevalence) in the 1st round of 2016 to 1395 cases (0.3% prevalence) in the 4th round of 2020 (Additional file 6: Table S5). With 2016 as reference, the percent reduction of malaria prevalence was estimated at 22.6% in 2017 (p < 0.001) and reached 75% in 2020 (p < 0.001) (Table 3). The effectiveness of SMC ranged from 76.6% for the second round to 96.2% for the fourth round in comparison with the first round.
According to the years of use, the effectiveness of SMC ranged from 1.5% in 2014 to 69.7% in 2020 in comparison with year 2013 (Table 4). According to the rounds, that effectiveness ranged from 68.2% for the second round to 96% for the 4th round in comparison with first round. There was also a heterogeneity in effectiveness between districts (e.g., Cinkassé, Kpendjal, Tandjoaré, Oti, Tone), or regions (Fig. 2, Additional file 6: Table S5, Additional file 1: Fig. S1). One interesting result is that rebounds were observed each year at the 1st round of SMC (Fig. 3).
Changes in malaria prevalence from 2013 to 2020 by year and round in whole Togo. Prevalence is defined as the number of children with malaria (children with positive ‘rapid diagnostic test’ (RDT) plus children already treated for malaria) divided by the number of children identified in the eligible age range
Changes in malaria prevalence (%) by region, year and round in Togo from 2013 to 2020 in Savanes region and from 2016 to 2020 in Central and Kara regions. Prevalence is defined as the number of children with malaria (children with positive ‘rapid diagnostic test’ (RDT) plus children already treated for malaria) divided by the number of children identified in the eligible age range
Discussion
Evaluating the effectiveness of strategies of fight against malaria allow health authorities to know the real impact of each strategy and make decisions relative to its sustainability and generalizability. The present results from Togo report reductions in malaria cases in children less than five wherever (all districts and all health regions) and whenever (all rounds and all years) SMC strategy was used.
Before 2013, the year of implementation of SMC in Togo (2013), there were frequent upsurges in malaria cases during the rainy seasons, especially among children under five. Indeed, in a recent study on malaria-related morbidity and mortality trends in Togo from 2008 to 2017 [12], morbidity tended to rise throughout Togo despite intensifications of various strategies and interventions. The present study shows that, since the start of SMC, there were only occasional fluctuations in malaria cases suggesting a decrease in the prevalence of malaria and a success of SMC. This is in agreement with: (i) fewer admissions of children under five to hospital for malaria during the rainy seasons (NMCP internal reports); and (ii) a rebound in malaria cases before each SMC yearly campaign.
Currently, there is no well-established way to estimate SMC effectiveness. The decrease in the prevalence of malaria cases as a function of time may be interpreted as an indication of SMC effectiveness, especially that, in the present study: (i) the coverage rate over time remained rather stable; (ii) SMC drug quality was ascertained by the PNLP; (iii) children identification system did not change; and, (iv) several major determinants of malaria transmission (incl. rainfall patterns, antivector fight) remained practically the same in SMC-targeted areas. Nevertheless, another way of estimating SMC effectiveness would consist in examining malaria incidence among non-targeted children (aged 6–10 years) per round and year. This is worth being implemented and its results compared with those of the current approach.
The specialized literature does not mention yet studies of SMC effectiveness outside Africa. In Africa, most studies on SMC were carried out in sub-Saharan West and Central Africa [11, 17,18,19,20,21] and concerned mostly limited areas (few villages or few districts) [11, 14, 15, 22,23,24,25,26]. The present study is most probably the first in Togo to evaluate the effectiveness of SMC strategy in children since its inception in that country, with one major asset that it was exhaustive over all health facilities of all districts where SMC was used. Apparently, a comparable exhaustiveness was seen only in Nigeria and Ghana [27, 28]. Here, it is worth mentioning that, among the strategies the Togolese NMCP has already applied to fight against malaria (insecticide nets and access to information, diagnostic, and treatment), SMC was the latest and had to be implemented according to the WHO's conditions regarding the sites (regions of high seasonal malaria transmission), the incidence (> 60% annual incidence), the morbidity (most morbidity in children), and anti-malarial drug efficacy (SP and AQ). Thus, at the time of the study, only Togolese Savanes, Kara, and Centrale regions met those criteria and were the sites of the present study. In the future, other sites will be eligible and the object of similar exhaustive investigations.
The results on SMC reported here are close to results of other studies found in the literature. Regarding morbidity and mortality, in December 2020, a large-scale observational study conducted in seven African countries (Burkina Faso, Gambia, Guinea, Mali, Niger, Nigeria, and Chad) [21] demonstrated that SMC was efficient in preventing morbidity and mortality from malaria in all seven countries. Precisely, in 2015 and 2016, nearly 12.5 and 25 million monthly SMC treatments were administered to nearly 3.6 and 7.6 million target children, respectively. The average monthly coverages were 76.4% in 2015 and 74.8% in 2016. The safety reports mentioned only 36 serious adverse reactions but no severe skin reaction. The efficacy of SMC was estimated at 88.2% over 28 days and the reduction of the number of malaria confirmed cases ranged from 25.5% (in Nigeria) to 55.2% (in Gambia). In Burkina Faso and Gambia, during the period of high transmission, SMC was respectively associated with 42.4% and 56.6% reductions in the number of deaths from malaria in hospital. Several other studies carried out in Africa have also demonstrated that SMC was well tolerated and helped reducing malaria transmission [13, 14].
In Togo, the interesting results obtained in the present study regarding malaria morbidity cannot be exclusively attributed to SMC; they result most probably from a combination of several concurrent preventive and curative interventions. Showing a SMC-specific efficiency requires conducting a clinical trial or a case–control study. Nevertheless, one asset of the present study is that 7,971,877 treatments (SP + AQ) could be administered to a target population of 8,129,668 children identified between 2013 and 2020. This 98% average coverage rate (WHO’s minimum: 95%) is the result of a combination of several organizational factors: (i) a thorough planning; (ii) a specific training of the CHWs and other actors of the campaigns; (iii) a social mobilization to maximize the contributions of the families; (iv) a door-to-door drug administration strategy implemented by CHWs with good knowledge of their areas (and even of the families) and eager to ensure SMC of nearly all identified children; (v) the use a specific card per child to mention the administration of the doses needed and a specific register per CHW to keep all needed information on drug administration; (vi) systematic surveys after each round to check whether all identified children were actually and adequately treated; (vii) surveys to check whether implementation improvements were needed in areas where the objectives were not met; and, (viii) appropriate monitoring, supervision, and coordination of all actors. Another asset is the existence of registries for malaria cases and deaths that make it possible to assess the impact of a set of interventions (including SMC).
The interest and reliability of the present results are most probably linked with the tireless and successful efforts of several actors on the field; mainly, committed CHWs and active social partners (incl. media representatives, community leaders, religious leaders, town criers). These efforts are important to make Togo join the States committed to fighting against malaria through SMC—among other strategies. The visibility of the efforts of all people engaged in that fight (from city criers to NMCP researchers and executives) is important to continue and overcome a number of still recurrent difficulties (at least in Togo): (i) shortage of significant financial resources to cover material and personnel costs; (ii) irregular coverage of target populations over time; (iii) ensuring less SMC rounds than recommended over certain years (2013, 2014); and (iv) lack of surveillance of parasite resistance against SP or AQ [29]. Incidentally, these difficulties might have underestimated the effectiveness of SMC on some occasions and in some circumstances.
Maximizing SMC efficiency requires mobilizing all local resources, looking for additional partners, and overcoming difficulties of access to either the territories or the populations during the rainy seasons (incl. muddy roads, busy farmers). One solution is to decentralize SMC and implement it in the community by the community. An additional solution is to increase the level of adherence of the population to SMC and support the surveillance systems.
Finally, SMC could have broader benefits if it could be: (i) widened to children over five because they are an important parasite reservoir [21]; and (ii) extended to areas less subject to malaria seasonal transmission.
Conclusion
The implementation of SMC in part of Togo between 2013 and 2020 has contributed to a reduction of malaria morbidity through a very high coverage rate that should be carefully monitored, sustained, and even increased and extended. This requires finding additional economic international partners of the NMCP and involving more national actors from the government, the private sector, and the civil society.
Availability of data and materials
Not applicable.
References
World Health Organization. Global Malaria Programme. World malaria report 2020: 20 years of global progress and challenges. Geneva: World Health Organization; 2020. p. 299.
WHO. World malaria report 2016. Geneva, World Health Organization, 2016. https://www.mmv.org/sites/default/files/uploads/docs/publications/World_Malaria_Report_2016.pdf. Accessed 6 July 2021.
World Health Organization. Policy recommendation: seasonal malaria chemoprevention (SMC) for Plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. Geneva: World Health Organization; 2012.
Konaté AT, Yaro JB, Ouédraogo AZ, Diarra A, Gansané A, Soulama I, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Burkina Faso: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8: e1000408.
Bojang K, Akor F, Bittaye O, Conway D, Bottomley C, Milligan P, et al. A randomised trial to compare the safety, tolerability and efficacy of three drug combinations for intermittent preventive treatment in children. PLoS ONE. 2010;5: e11225.
Cissé B, Sokhna C, Boulanger D, Milet J, el Bâ H, Richardson K, et al. Seasonal intermittent preventive treatment with artesunate and sulfadoxine-pyrimethamine for prevention of malaria in Senegalese children: a randomised, placebo-controlled, double-blind trial. Lancet. 2006;367:659–67.
Dicko A, Sagara I, Sissoko MS, Guindo O, Diallo AI, Kone M, et al. Impact of intermittent preventive treatment with sulphadoxine-pyrimethamine targeting the transmission season on the incidence of clinical malaria in children in Mali. Malar J. 2008;7:123.
Kweku M, Liu D, Adjuik M, Binka F, Seidu M, Greenwood B, et al. Seasonal intermittent preventive treatment for the prevention of anaemia and malaria in Ghanaian children: a randomized, placebo controlled trial. PLoS ONE. 2008;3: e4000.
Sesay S, Milligan P, Touray E, Sowe M, Webb EL, Greenwood BM, et al. A trial of intermittent preventive treatment and home-based management of malaria in a rural area of The Gambia. Malar J. 2011;10:2.
Wilson AL, IPTc Taskforce. A systematic review and meta-analysis of the efficacy and safety of intermittent preventive treatment of malaria in children (IPTc). PLoS One. 2011;6:e16976.
Meremikwu MM, Donegan S, Sinclair D, Esu E, Oringanje C. Intermittent preventive treatment for malaria in children living in areas with seasonal transmission. Cochrane Database Syst Rev. 2012;2012:CD003756.
Bakai TA, Thomas A, Iwaz J, Atcha-Oubou T, Tchadjobo T, Khanafer N, et al. Changes in registered malaria cases and deaths in Togo from 2008 to 2017. Int J Infect Dis. 2020;101:298–305.
Issiaka D, Barry A, Traore T, Diarra B, Cook D, Keita M, et al. Impact of seasonal malaria chemoprevention on hospital admissions and mortality in children under 5 years of age in Ouelessebougou, Mali. Malar J. 2017;16:325.
Cissé B, Ba EH, Sokhna C, NDiaye JL, Gomis JF, Dial Y, et al. Effectiveness of seasonal malaria chemoprevention in children under ten years of age in Senegal: a stepped-wedge cluster-randomised trial. PLoS Med. 2016;13:e1002175.
Cairns ME, Sagara I, Zongo I, Kuepfer I, Thera I, Nikiema F, et al. Evaluation of seasonal malaria chemoprevention in two areas of intense seasonal malaria transmission: Secondary analysis of a household-randomised, placebo-controlled trial in Houndé District, Burkina Faso and Bougouni District. Mali PLoS Med. 2020;17: e1003214.
Tagbor H, Antwi GD, Acheampong PR, Bart Plange C, Chandramohan D, Cairns M. Seasonal malaria chemoprevention in an area of extended seasonal transmission in Ashanti, Ghana: an individually randomised clinical trial. Trop Med Int Health. 2016;21:224–35.
Noor AM, Kibuchi E, Mitto B, Coulibaly D, Doumbo OK, Snow RW. Sub-national targeting of seasonal malaria chemoprevention in the Sahelian countries of the Nouakchott Initiative. PLoS ONE. 2015;10: e0136919.
Coldiron ME, Assao B, Langendorf C, Sayinzoga-Makombe N, Ciglenecki I, de la Tour R, et al. Clinical diagnostic evaluation of HRP2 and pLDH-based rapid diagnostic tests for malaria in an area receiving seasonal malaria chemoprevention in Niger. Malar J. 2019;18:443.
Cairns M, Roca-Feltrer A, Garske T, Wilson AL, Diallo D, Milligan PJ, et al. Estimating the potential public health impact of seasonal malaria chemoprevention in African children. Nat Commun. 2012;3:881.
Bâ EH, Pitt C, Dial Y, Faye SL, Cairns M, Faye E, et al. Implementation, coverage and equity of large-scale door-to-door delivery of Seasonal Malaria Chemoprevention (SMC) to children under 10 in Senegal. Sci Rep. 2018;8:5489.
ACCESS-SMC Partnership. Effectiveness of seasonal malaria chemoprevention at scale in west and central Africa: an observational study. Lancet. 2020;396:1829–40.
Konaté D, Diawara SI, Touré M, Diakité SAS, Guindo A, Traoré K, et al. Effect of routine seasonal malaria chemoprevention on malaria trends in children under 5 years in Dangassa, Mali. Malar J. 2020;19:137.
Ndiaye JLA, Ndiaye Y, Ba MS, Faye B, Ndiaye M, Seck A, et al. Seasonal malaria chemoprevention combined with community case management of malaria in children under 10 years of age, over 5 months, in south-east Senegal: a cluster-randomised trial. PLoS Med. 2019;16: e1002762.
Chatio S, Ansah NA, Awuni DA, Oduro A, Ansah PO. Community acceptability of Seasonal Malaria Chemoprevention of morbidity and mortality in young children: a qualitative study in the Upper West Region of Ghana. PLoS ONE. 2019;14: e0216486.
Issiaka D, Barry A, Traore T, Diarra B, Cook D, Keita M, et al. Impact of seasonal malaria chemoprevention on hospital admissions and mortality in children under 5 years of age in Ouelessebougou, Mali. Malar J. 2017;16:325.
Druetz T, Corneau-Tremblay N, Millogo T, Kouanda S, Ly A, Bicaba A, et al. Impact evaluation of seasonal malaria chemoprevention under routine program implementation: a quasi-experimental study in Burkina Faso. Am J Trop Med Hyg. 2018;98:24–33.
Ambe JP, Balogun ST, Waziri MB, Nglass IN, Saddiq A. Impacts of seasonal malaria chemoprevention on malaria burden among under five-year-old children in Borno State, Nigeria. J Trop Med. 2020;2020:9372457.
Nonvignon J, Aryeetey GC, Issah S, Ansah P, Malm KL, Ofosu W, et al. Cost-effectiveness of seasonal malaria chemoprevention in upper west region of Ghana. Malar J. 2016;15:367.
Dicko A, Diallo AI, Tembine I, Dicko Y, Dara N, Sidibe Y, Santara G, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Mali: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8: e1000407.
Acknowledgements
The authors acknowledge the field activities of the agents of the National Malaria Control Program (NMCP) of Togo who collected the data processed here.
Funding
This work was supported by EPIMOD company, Association Nationale de la Recherche et de la Technologie (ANRT) [CIFRE Grant 2017/1805)], and Auvergne-Rhône-Alpes region (Grant 19 003 721 01).
Author information
Authors and Affiliations
Contributions
TAB, MR and NV designed the study. TAB, TA and TT collected the data. AT, NV and TAB analysed the data. TAB, MR and NV interpreted the results and wrote the manuscript. JI, TAB, MR, NV, and NK revised the manuscript until its final version. NV ensured the supervision of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests in relation with this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Heterogeneity of yearly and cycle seasonal malaria chemoprevention effects in the districts of Togo from 2016 to 2020. Deviation of each district from the average is represented for yearly and cycle effects. Districts below line 0 (Blitta, Oti, Sotouboua, Tchamba, and Tchaoudjo) showed better effectiveness of seasonal malaria chemoprevention than the average and districts above line 0 (Binah, Cinkasse, Dankpen, Kozah and Kpendjal) showed lower effectiveness.
Additional file 2: Table S1.
Participating health facilities in seasonal malaria chemoprevention districts, Togo, 2013–2020.
Additional file 3: Table S2.
Numbers of children identified in seasonal malaria chemoprevention zones, Togo, 2013–2020.
Additional file 4: Table S3.
Reasons for not administering seasonal malaria chemoprevention per district, Togo, 2013–2020.
Additional file 5: Table S4.
Side effects linked with seasonal malaria prevention drugs, Togo, 2013–2020.
Additional file 6: Table S5.
Number of malaria cases in seasonal malaria chemoprevention zones, Togo, 2013–2020.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bakai, T.A., Thomas, A., Iwaz, J. et al. Effectiveness of seasonal malaria chemoprevention in three regions of Togo: a population-based longitudinal study from 2013 to 2020. Malar J 21, 400 (2022). https://doi.org/10.1186/s12936-022-04434-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04434-w